It’s one of the first questions my patients ask: “Doctor, do I really need surgery? Can’t this be fixed with medication?” It’s a valid and important question. As a medical professional, my goal is to find the most effective and least invasive treatment for you.
The truth is, there is a time and place for medical treatment, but its effectiveness is tied to a very specific and limited window of opportunity. Here, I’ll explain when medication can work, and when surgery becomes the only definitive, permanent solution.
The Observation Period: Diagnosing Transient vs. Persistent Disease
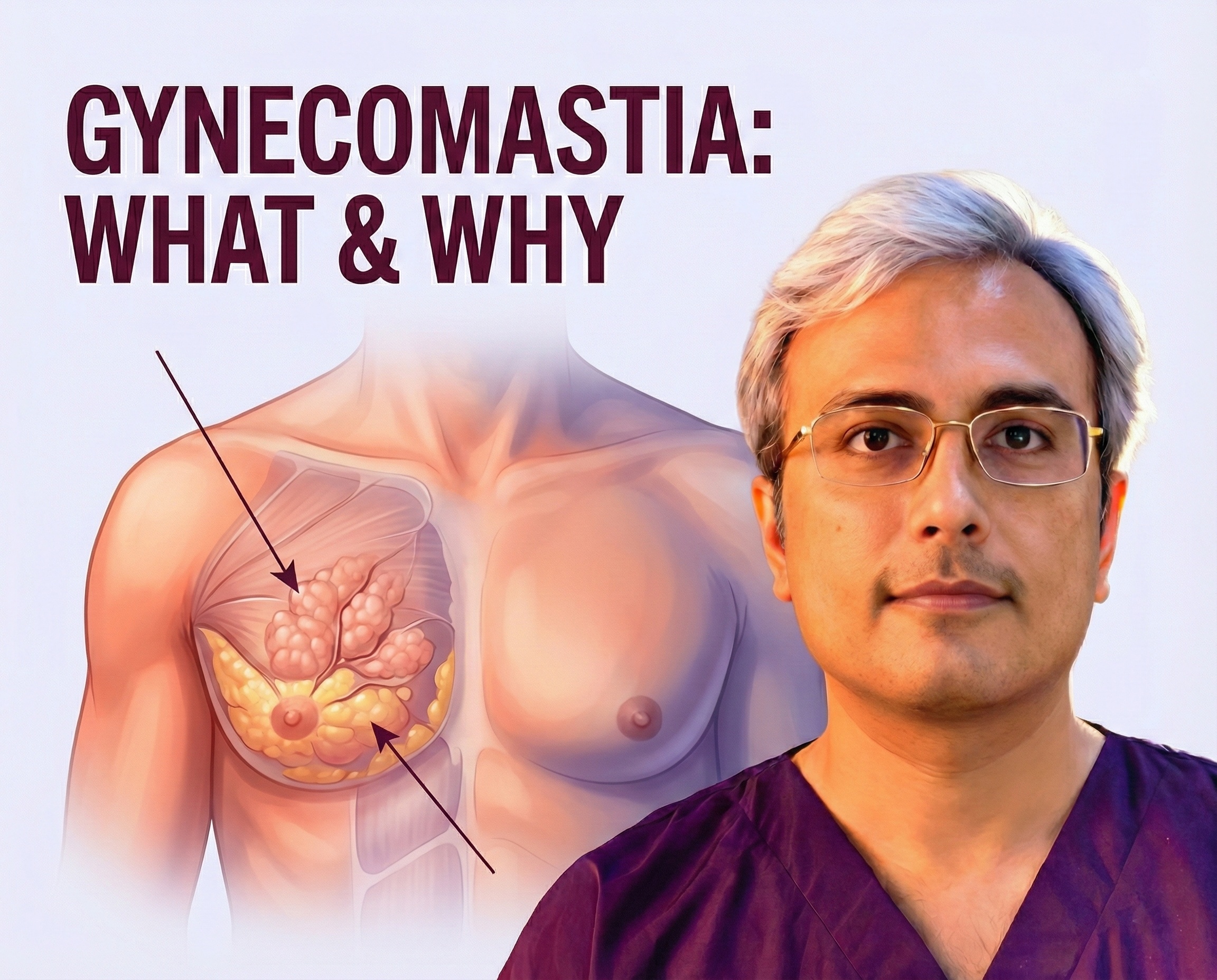
For many individuals, particularly those experiencing pubertal gynecomastia, male breast enlargement is a temporary, physiological condition. In cases where the workup is benign, observation and reassurance are usually sufficient, given that the condition is usually self-limiting.
Adolescent Window
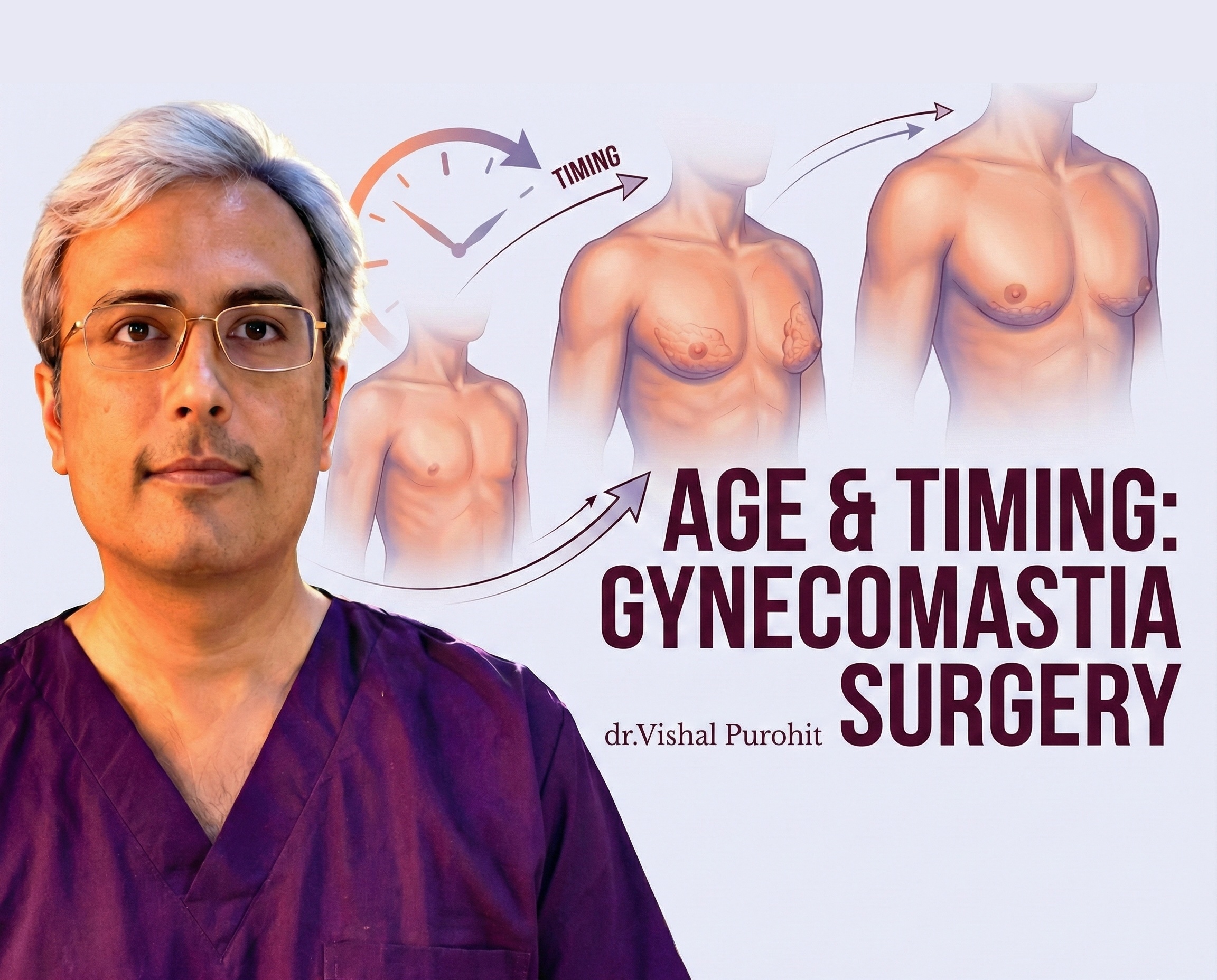
Physiologic gynecomastia, which occurs during puberty, resolves spontaneously within 1 to 3 years in 75–90% of adolescents. In more than 75% of cases, the condition goes away in 18 months. We explore this in detail in our guide on the proper age and timing for gynecomastia surgery.
Pathological Cause Correction:
If a specific, underlying cause of gynecomastia (such as a drug or hormonal disorder) is identified, treating that disorder is generally sufficient to cause regression of gynecomastia. Treatment of underlying disorders or withdrawal of causal drugs should be used in selected patients who are symptomatic or have recent-onset gynecomastia.
A thorough clinical evaluation is needed to gain a clear understanding of the condition and rule out other health issues.
The Crucial Time Limit:
If the condition persists for more than 12 months, the tissue often becomes dense and fibrotic. Gynecomastia is unlikely to regress spontaneously once it is long-standing.
An algorithm for the evaluation and treatment suggests observation and reassurance if the workup is benign, but if the condition persists and medical therapy does not work, surgery should be considered.
Gynecoamstia Medical Treatment: Efficacy and Counter-Arguments
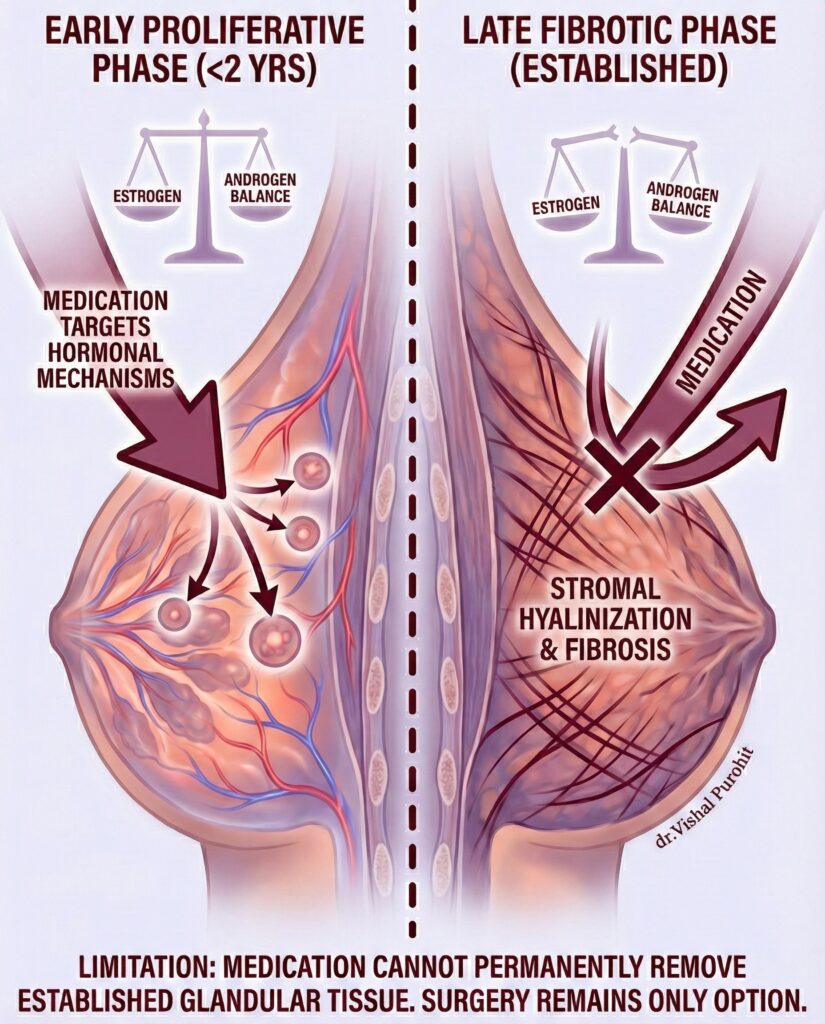
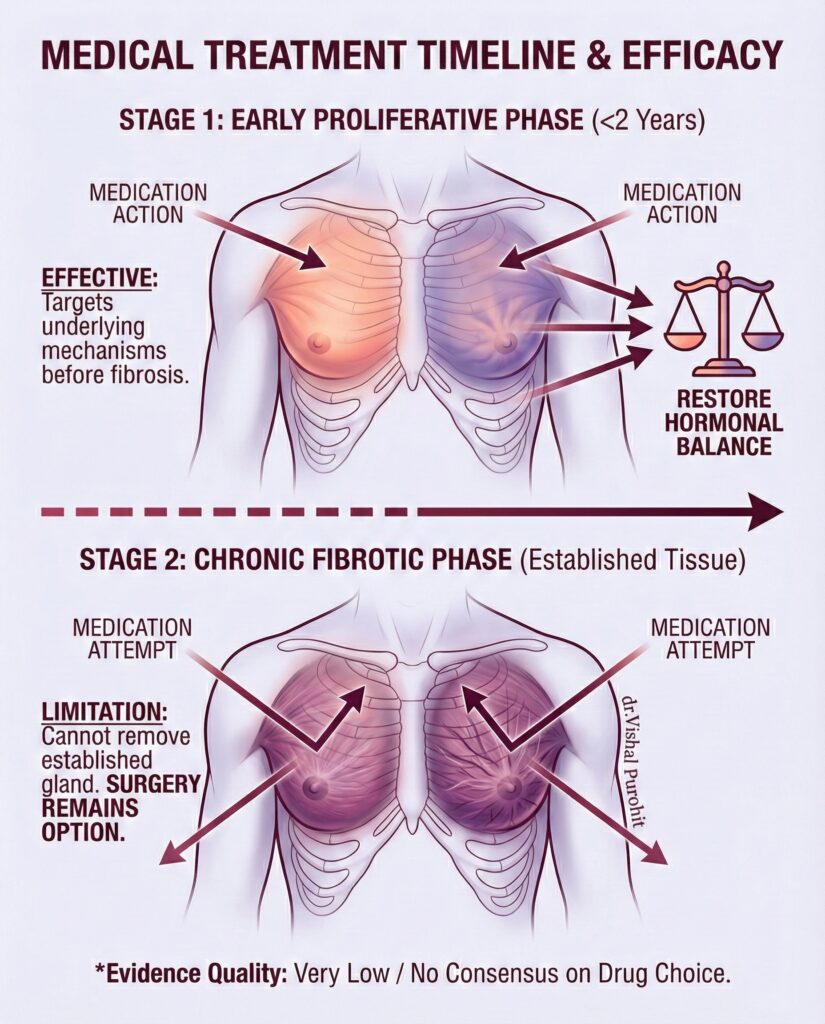
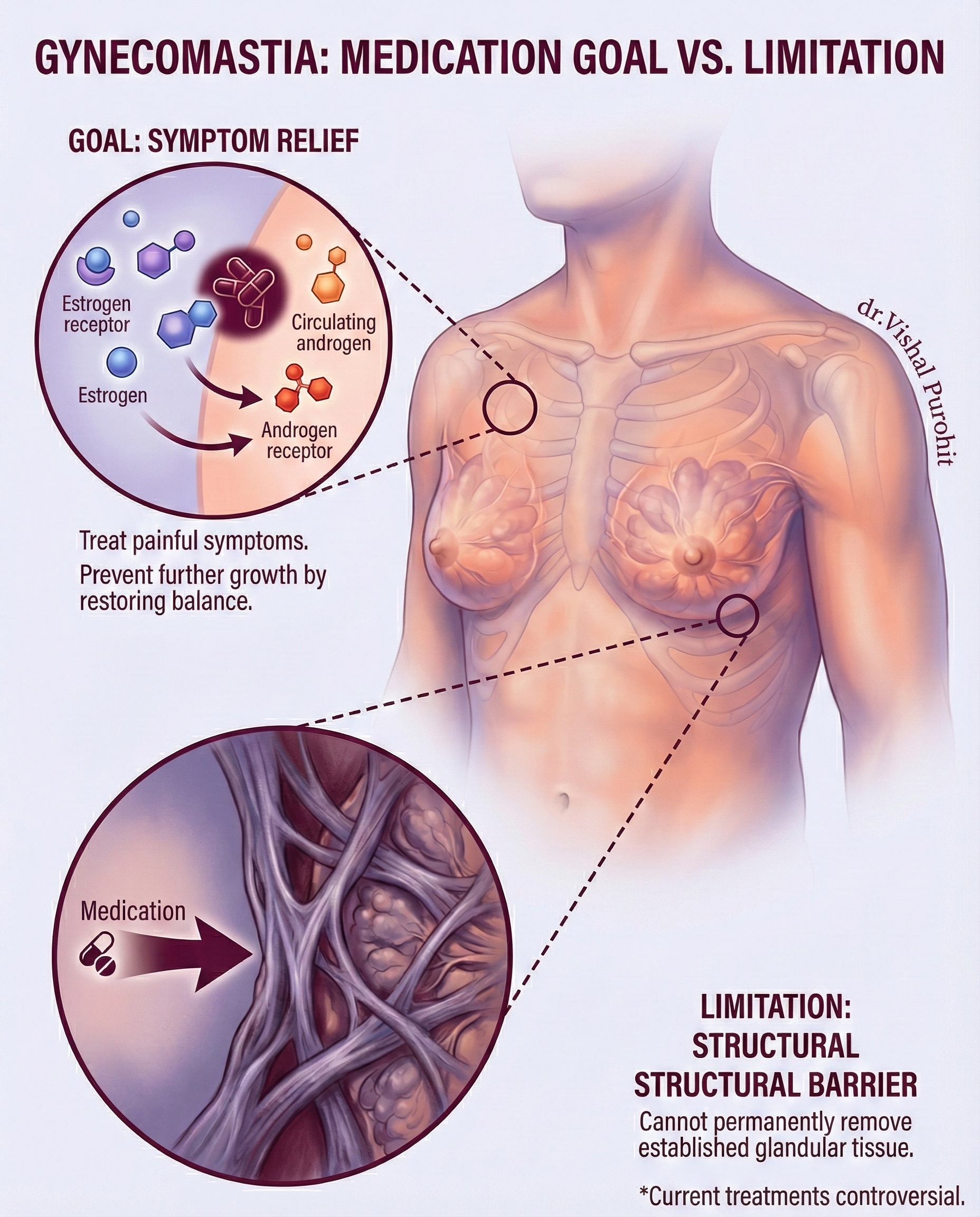
Medical treatment aims to restore the estrogen-to-androgen balance in the body, but it is only effective during the early proliferative phase, before stromal hyalinization and fibrosis.
When medical treatment is pursued (typically within that first two-year window) for gynecomastia, the medications prescribed directly target the underlying hormonal mechanisms that cause breast tissue proliferation, aiming to restore the balance between estrogen and androgen action.
Evidence Limitation, Pharmacology Offers Gynecomastia Symptom Relief, Not Permanent Cure
It is crucial to understand the fundamental limitation: medication generally addresses the symptoms or prevents further growth of gynecomastia, but it cannot permanently remove established glandular tissue.
- Goal of Medication: Medical treatment may be used to treat cosmetically disturbing or painful gynecomastia.
- Limitation: Medication cannot get rid of the breast tissue permanently once the gynecomastia gland is well-formed. Surgery remains the only option when chronic glandular tissue is present.
Medical treatment is currently controversial. There is no consensus regarding the drug of choice or the optimal duration of treatment for gynecomastia.
Furthermore, literature data on the efficacy of medical treatment for gynecomastia is often limited to small case series and case reports without control groups. A systematic review found that studies concerning pharmacological treatment for gynecomastia were of very low quality of evidence.
If medical management fails to reduce the size after a set period, we will then assess your eligibility for surgery.
Specific Drug Classes Used in Treatment
Medications are prescribed to disrupt the estrogenic signals that drive breast tissue growth.
Anti-oestrogens such as Tamoxifen are effective in reducing breast pain and size. Danazol therapy is effective in 80% of patients and can be repeated for non-responders, but Tamoxifen, while effective, is associated with a high relapse rate.
Clomiphene, another anti-oestrogen, proved unsuccessful and was associated with adverse side-effects. Aromatase inhibitors, which prevent the conversion of androgens to estrogens, should alleviate gynecomastia.
Gynecomastia can respond well to medical treatment, but it is usually effective only when done within the first two years after the start of male breast enlargement. Medical treatment of gynecomastia that has persisted beyond two years is often ineffective.
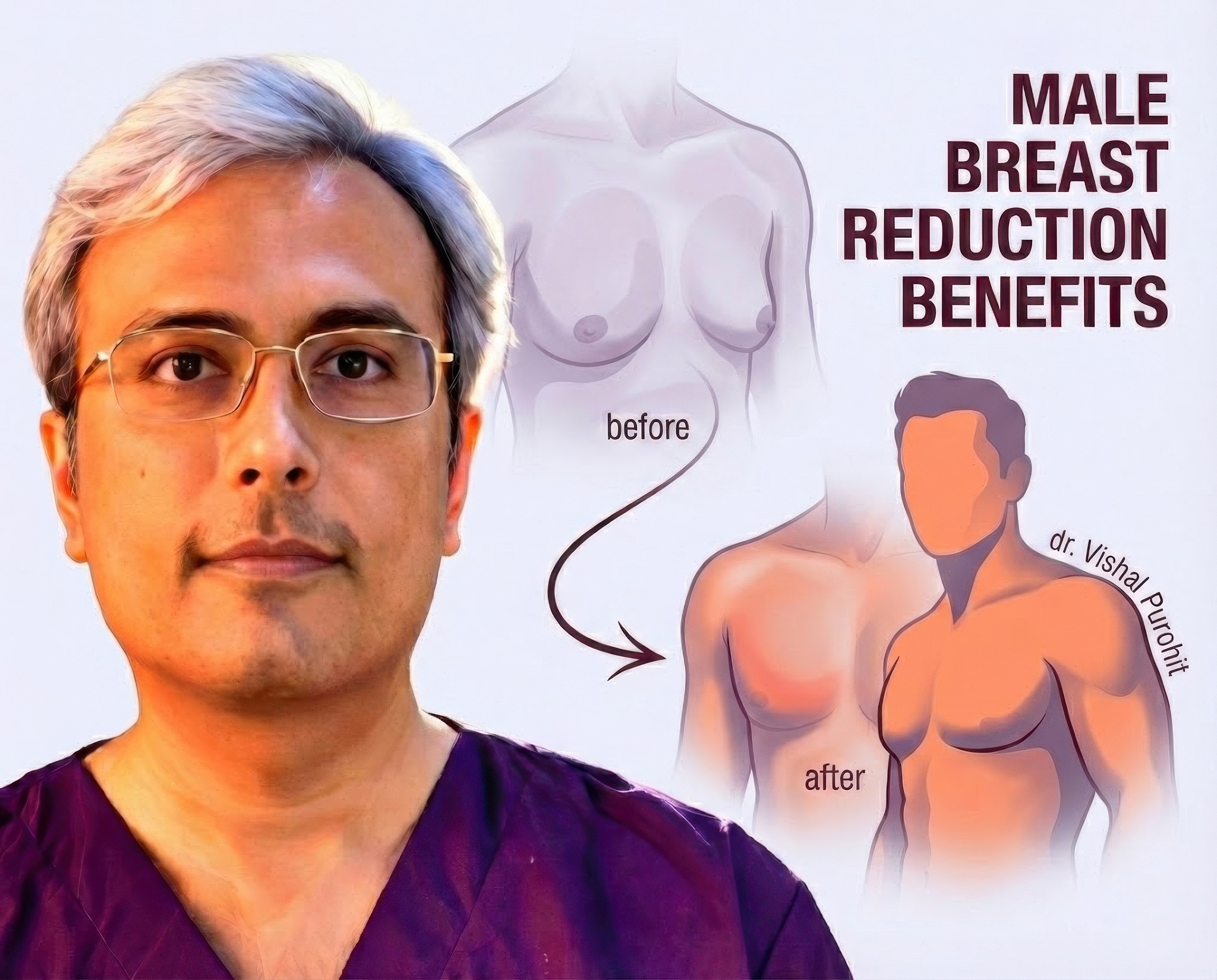
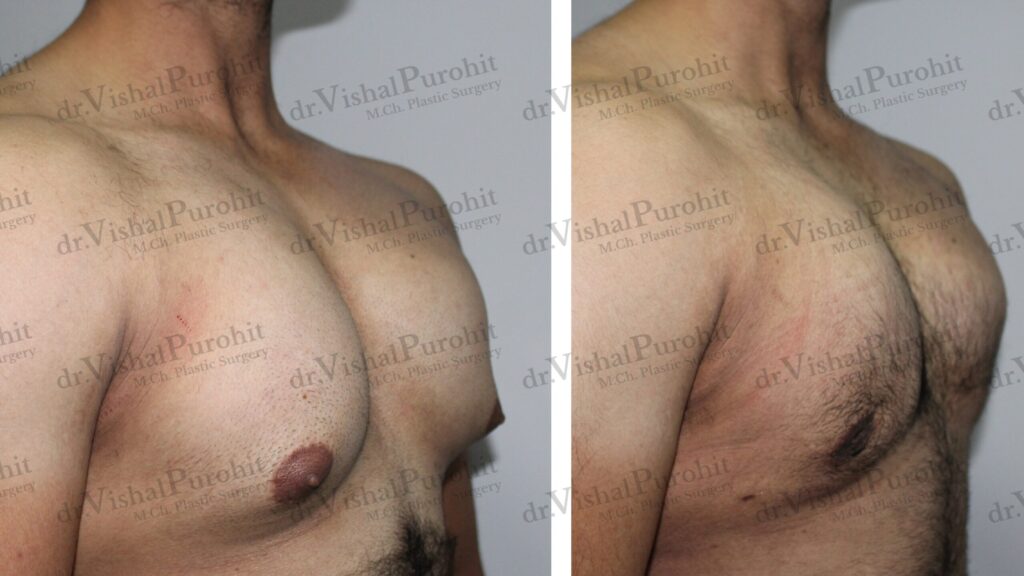
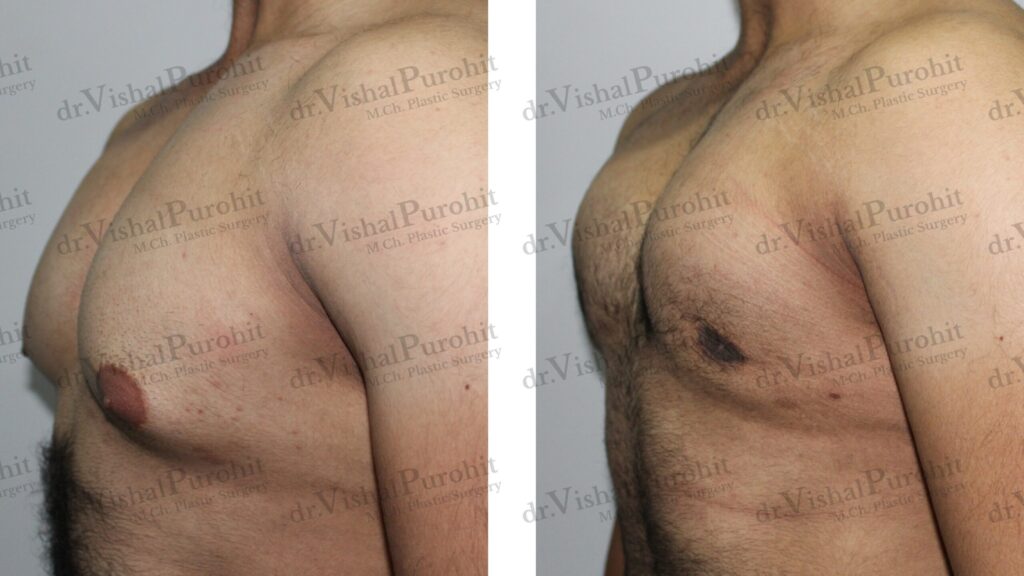
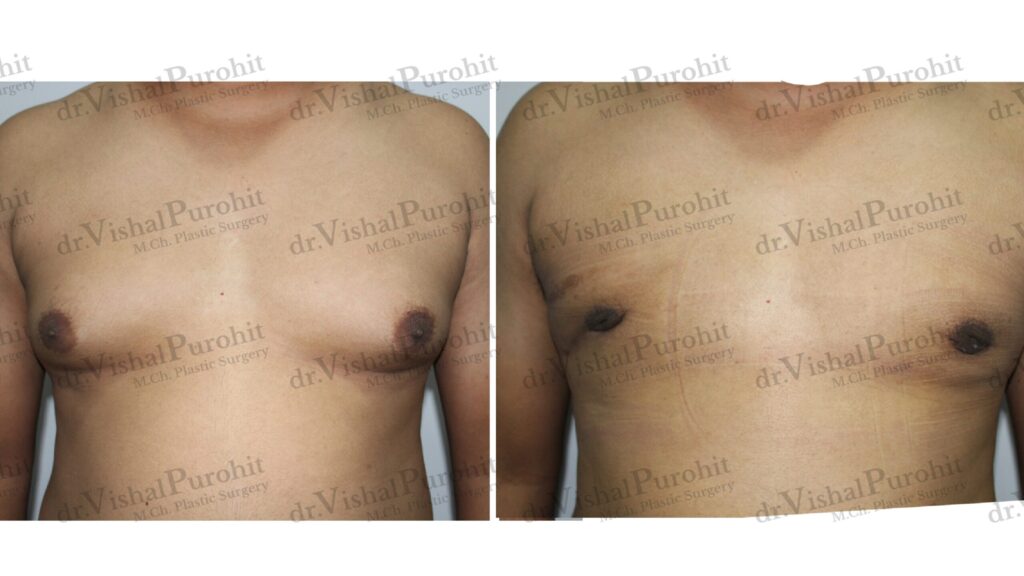
If chronic gynecomastia does not respond to medical treatment, the surgical removal of glandular tissue is usually required. Surgery remains the only option for male breast reduction when chronic glandular tissue is present.
If your enlargement has lasted for more than two years, the window for effective medical treatment has likely closed. This is the point where we transition from temporary options to a permanent, contoured chest as part of a comprehensive Gynecomastia Treatment plan in Jaipur.
Frequently Asked Questions
Can gynecomastia be treated effectively with medications alone?
Gynecomastia can be treated effectively with medications alone, but only if the intervention occurs during the early, acute phase of the condition. This phase, often called the “proliferation phase,” is characterised by active glandular growth and inflammation. Medical therapies have been found to be most effective during this proliferation phase, before the tissue undergoes structural changes.
The window of opportunity for medical treatment is relatively narrow. Generally, medication is effective only if started within the first 12 to 24 months of onset. During this period, the breast tissue is still responsive to hormonal manipulation. Once the condition has persisted beyond this timeframe, the stromal tissue typically becomes dense and fibrotic.
If the condition has been present for more than one year, the likelihood of success with medication drops significantly. Studies indicate that once fibrous Umbauprozesse (restructuring) or fibrosis occurs in the tissue, usually after 12 months, the tissue becomes inactive and largely unresponsive to drug therapy. At this chronic stage, the collagenous fibres become dense and hyalinized, making surgery the only definitive treatment option.
Therefore, while medications can be a successful first-line treatment for recent-onset gynecomastia, they are rarely effective for long-standing cases. If you have had enlarged breasts for several years, relying on medication alone will likely lead to frustration, and surgical removal of the glandular tissue will be required to achieve a flat chest.
Which medical treatments are commonly used for gynecomastia, and when are they effective?
The most commonly used medical treatments for gynecomastia are Selective Estrogen Receptor Modulators (SERMs), such as Tamoxifen and Raloxifene, and occasionally androgens like Danazol. These medications work by blocking the effects of estrogen on the breast tissue or by altering the hormonal environment to favour androgens. Tamoxifen, for instance, has been shown to be effective in up to 90% of cases for the resolution of gynecomastia when used in doses of 10–20 mg daily.
Danazol, a weak androgen, has also been used with success. In controlled trials, Danazol was shown to provide effective control of symptoms and reduce breast size in about 80% of patients. It is particularly effective in reducing breast tenderness. However, while Danazol is licensed for this use in some regions like the UK, Tamoxifen is often used off-label but is frequently preferred due to its safety profile and effectiveness in reducing breast volume.
Another class of drugs utilised includes Aromatase Inhibitors (AIs) like Anastrozole, which prevent the conversion of androgens into estrogens. While theoretically sound, AIs have generally been less effective than antiestrogens like Tamoxifen in treating pubertal gynecomastia and are often reserved for specific conditions like Peutz-Jeghers syndrome.
These treatments are most effective when the gynecomastia is caused by a reversible hormonal imbalance or drug induction and is treated early. For example, if gynecomastia is induced by anti-androgen therapy for prostate cancer, Tamoxifen has been advocated as a prophylactic or treatment measure. However, once the tissue becomes fibrotic, these medications lose their efficacy.
How do I know whether my gynecomastia will respond to medical therapy or require surgery?
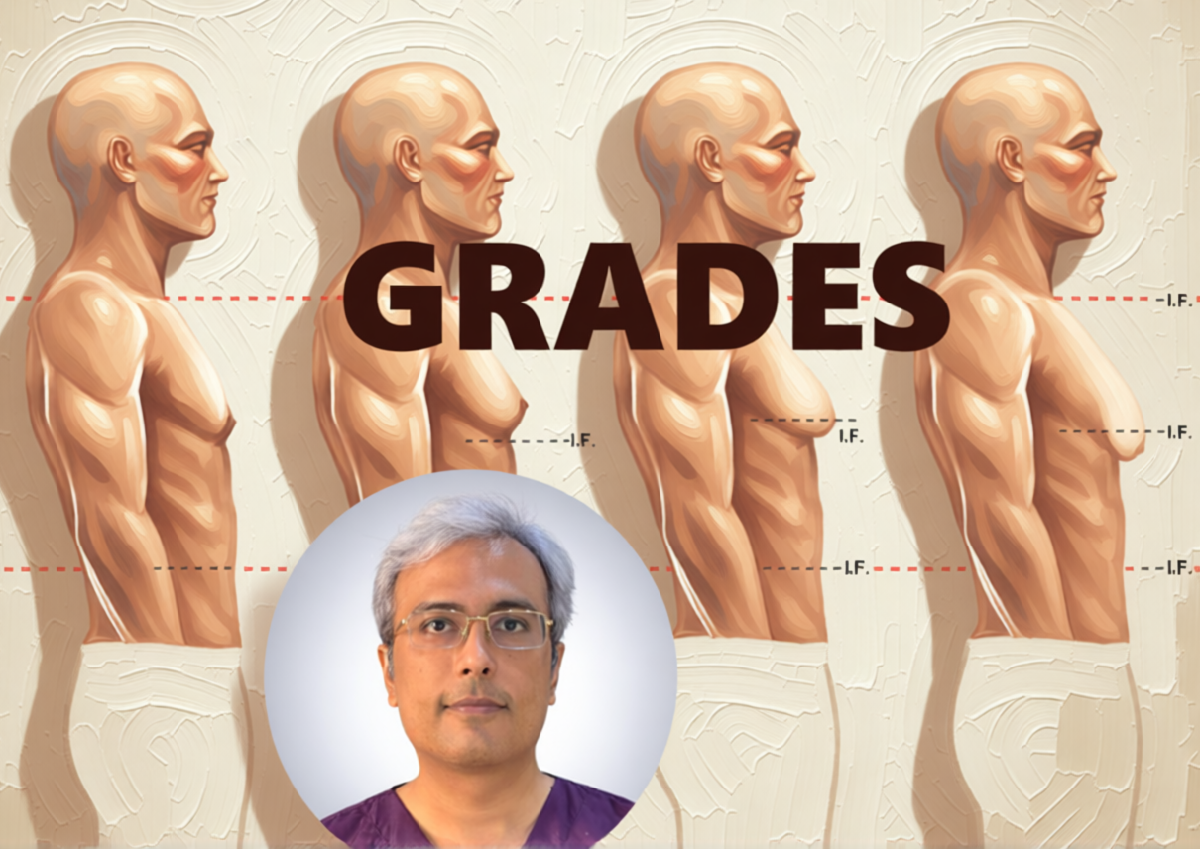
You can generally determine if your gynecomastia will respond to medical therapy based on the duration of the condition and the texture of the breast tissue. If your breast enlargement appeared recently (less than 12 to 24 months ago) and the tissue feels soft and tender, it is likely in the proliferative phase. In this stage, the tissue is biologically active and has a higher chance of regressing with medical management.
Conversely, if you have had the condition for more than two years, or if the breast tissue feels firm, rubbery, and painless, it has likely entered the fibrotic phase. Once this stromal fibrosis becomes the predominant feature, the tissue is irreversible and will not respond to medication. At this point, the only way to remove the dense, fibrous tissue is through surgical excision.
Physical symptoms such as pain or tenderness (mastodynia) are also good indicators that the tissue is still active and potentially responsive to medication. Danazol and Tamoxifen are particularly noted for their ability to alleviate tenderness. If the pain has subsided and the mass has stabilised in size for a long period, surgery is usually the required path.
Ultimately, a consultation with a specialist is necessary to distinguish between the two phases. If clinical evaluation confirms that the medical treatment is effective for gynecomastia window has passed, you can save time and emotional energy by moving directly to surgical planning rather than attempting ineffective drug therapies.
Are there any risks or side effects associated with hormonal or medical treatment for gynecomastia?
Yes, hormonal and medical treatments for gynecomastia do carry risks and side effects, though they are generally considered safe for short-term use. For example, Danazol is associated with side effects such as weight gain, acne, and muscle cramps. Although it is effective, these androgenic side effects can be bothersome for some patients.
Tamoxifen, while effective and widely used, is not without risks. Common side effects include nausea and hot flashes. Furthermore, although it can resolve the condition, it is associated with a higher relapse rate compared to Danazol upon cessation of the drug. In rare cases, the use of SERMs has been associated with increased risks of deep vein thrombosis, though this is less common in healthy young males.
Aromatase inhibitors like Anastrozole can lead to decreased bone mineral density if used for prolonged periods, making them less favourable for developing adolescents. Additionally, their efficacy in reducing breast volume in pubertal gynecomastia has been shown to be lower than that of Tamoxifen.
It is also important to consider the psychological impact of prolonged, ineffective medical treatment. Relying on medication for a condition that has already become fibrotic can lead to extended periods of psychosocial distress. Therefore, the safety and efficacy of tamoxifen must always be weighed against the definitive and immediate results offered by surgery.
How long does it take to see results from medical treatment for gynecomastia?
When medical treatment is initiated in the appropriate candidate, results can typically be seen within 1 to 3 months. For example, treatments with Tamoxifen have shown regression of breast tissue and alleviation of pain within 3 to 9 months of therapy. If a specific drug is causing the gynecomastia, withdrawal of that drug usually leads to improvement within a few weeks.
If there is no significant reduction in breast size after 3 to 6 months of medical therapy, it is generally considered a treatment failure. Continued medical treatment beyond this point is rarely beneficial. In studies of Danazol, a standard course involves 6 weeks to several months; if no response is seen, the treatment is discontinued.
It is crucial to set a time limit for medical trials. Persisting with medication for years is not recommended due to the unknown long-term side effects and the low probability of success in chronic cases. If the condition does not resolve within this short therapeutic window, or if it has persisted for more than 2 years, surgery becomes the only useful treatment.
Therefore, patience is required, but it should be limited. If you do not see visible changes within the first few months of treatment, you should return to your physician to discuss surgical options to permanently resolve the issue.
Your Consultation in Jaipur
If you have tried medical treatments without success, or if your gynecomastia is chronic, it requires the definitive removal of the glandular tissue. I invite you to consult with my team in Jaipur to transition from temporary symptomatic relief to a permanent surgical solution.
To book your personalised, confidential consultation, please reach out to my team at Kalpana Aesthetics.
- Call or WhatsApp: 7718183535
- Visit Us: Kalpana Aesthetics, 2nd Floor, Jaipur Hospital, Mahaveer Nagar, Tonk Road, Jaipur
Disclaimer: The information provided on this webpage is for educational purposes only and does not constitute medical advice. The effectiveness of medical treatments for gynecomastia is highly variable and depends on the cause and duration of the condition. Do not start or stop any medication without consulting your doctor. Please consult with a qualified, board-certified plastic surgeon for a definitive diagnosis and treatment plan.