One of the first questions I hear during a consultation isn’t about the surgery itself—it is about the aftermath. “Doctor, will everyone know I had surgery? Will I have a big scar on my chest?”
This is a valid fear. You are choosing surgery to feel confident going shirtless, so trading “man boobs” for a visible, jagged scar defeats the purpose.
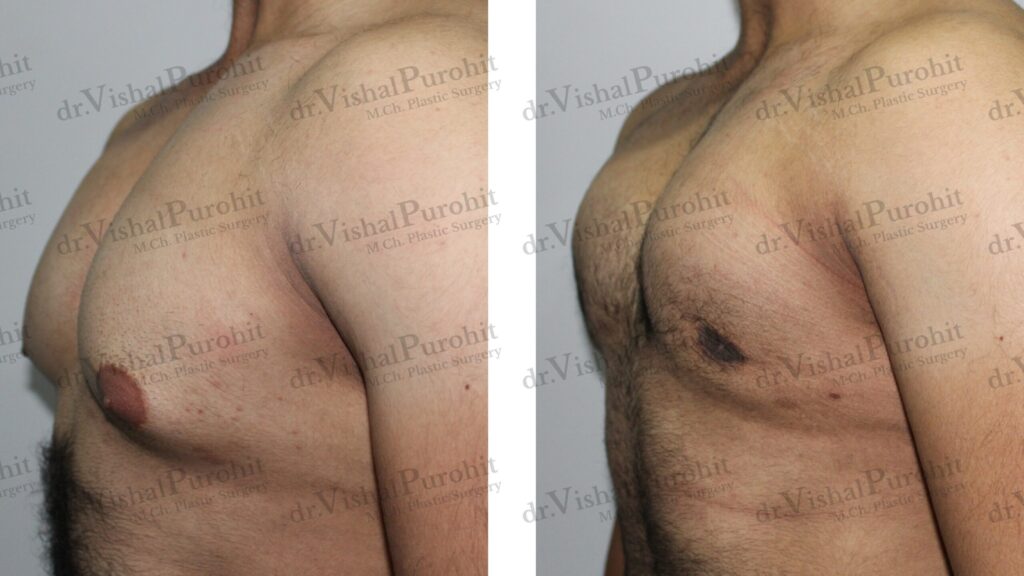
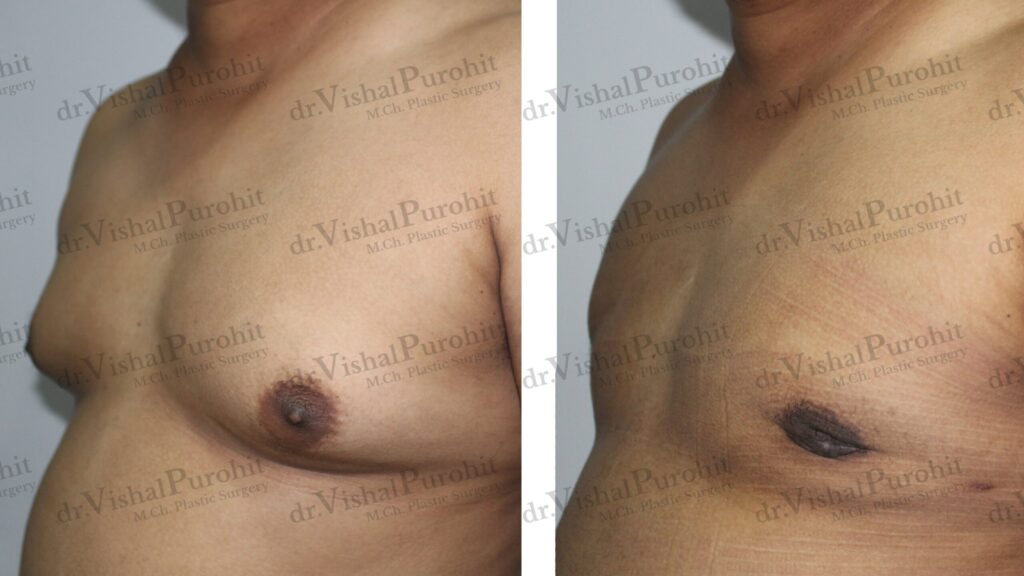
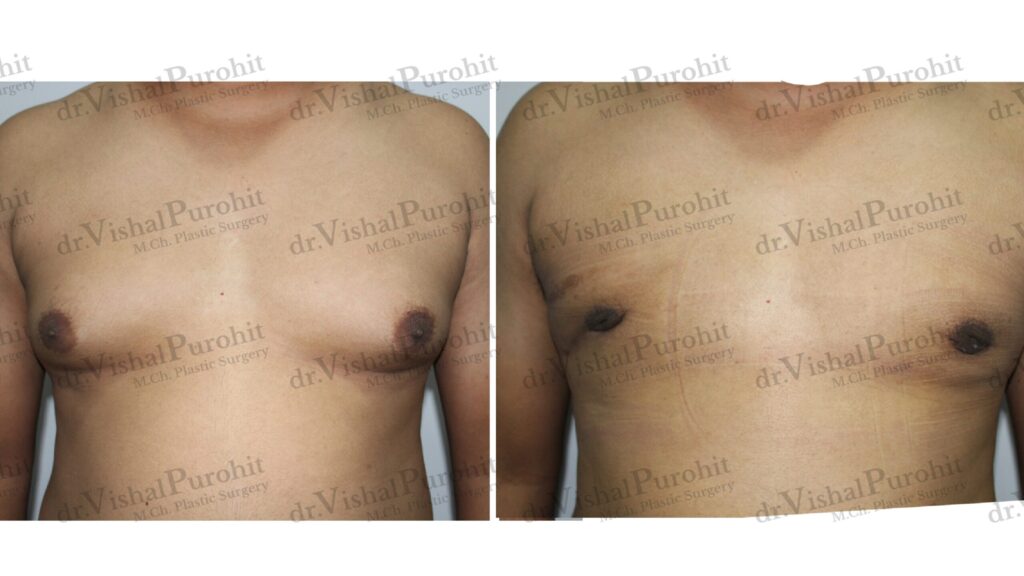
As a specialist in Gynecomastia Surgery in Jaipur, my goal is not just to remove the gland, but to leave your chest looking as if it was never touched. In this guide, I will explain the reality of scarring and the advanced “stealth incision” techniques we use to ensure your confidence remains scar-free.
The Reality: Does Surgery Leave Scars?
In plastic surgery, there is a saying: “Only a ghost leaves no tracks.” Technically, any time an incision is made in the skin, a scar is formed.
The appearance of the scar will fade significantly during the healing process, turning from red to a faint white line over 6-12 months.
However, there is a difference between a scar and a visible scar.
The goal of aesthetic male breast reduction is to place incisions in areas where they are naturally camouflaged by your body’s anatomy. When performed correctly by a board-certified surgeon, the resulting mark should be virtually imperceptible to the naked eye once healed.
The specific location of the incision depends largely on the gynecomastia surgical technique used, whether it is pure liposuction or open gland excision.
Strategic Incision Placement: The “Invisible” Technique
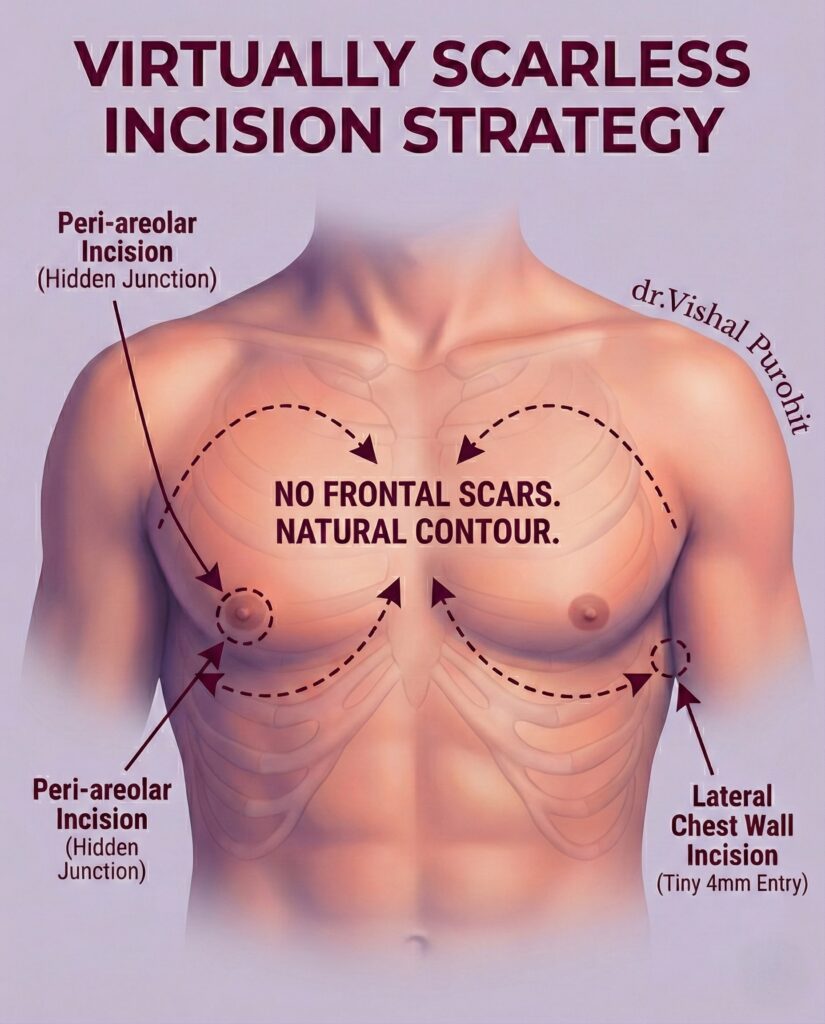
To ensure “scarless confidence,” we use specific anatomical borders to hide the entry points.
For Gland Excision (The Webster Incision)
When removing the firm glandular tissue, we typically use a Periareolar Incision.
- Location: The cut is made precisely along the lower border of the areola (the dark skin surrounding the nipple).
- The Camouflage: The scar sits exactly at the junction where the dark areolar skin meets the lighter chest skin. This natural colour transition masks the fine line, making it nearly invisible after a few months.
- Clinical Efficacy: While liposuction addresses fat, it is well-documented that liposuction alone usually will not fully correct the glandular component. Therefore, this hidden incision is often necessary to remove the tough, rubbery tissue that causes nipple puffiness.
For Liposuction (Fat Removal)
- Location: Tiny punctures (less than 4mm) are made in the armpit (axilla) or very low on the side of the chest.
- The Camouflage: These spots are hidden by the arms or the natural shadows of the body.
Scars by Grade: What to Expect
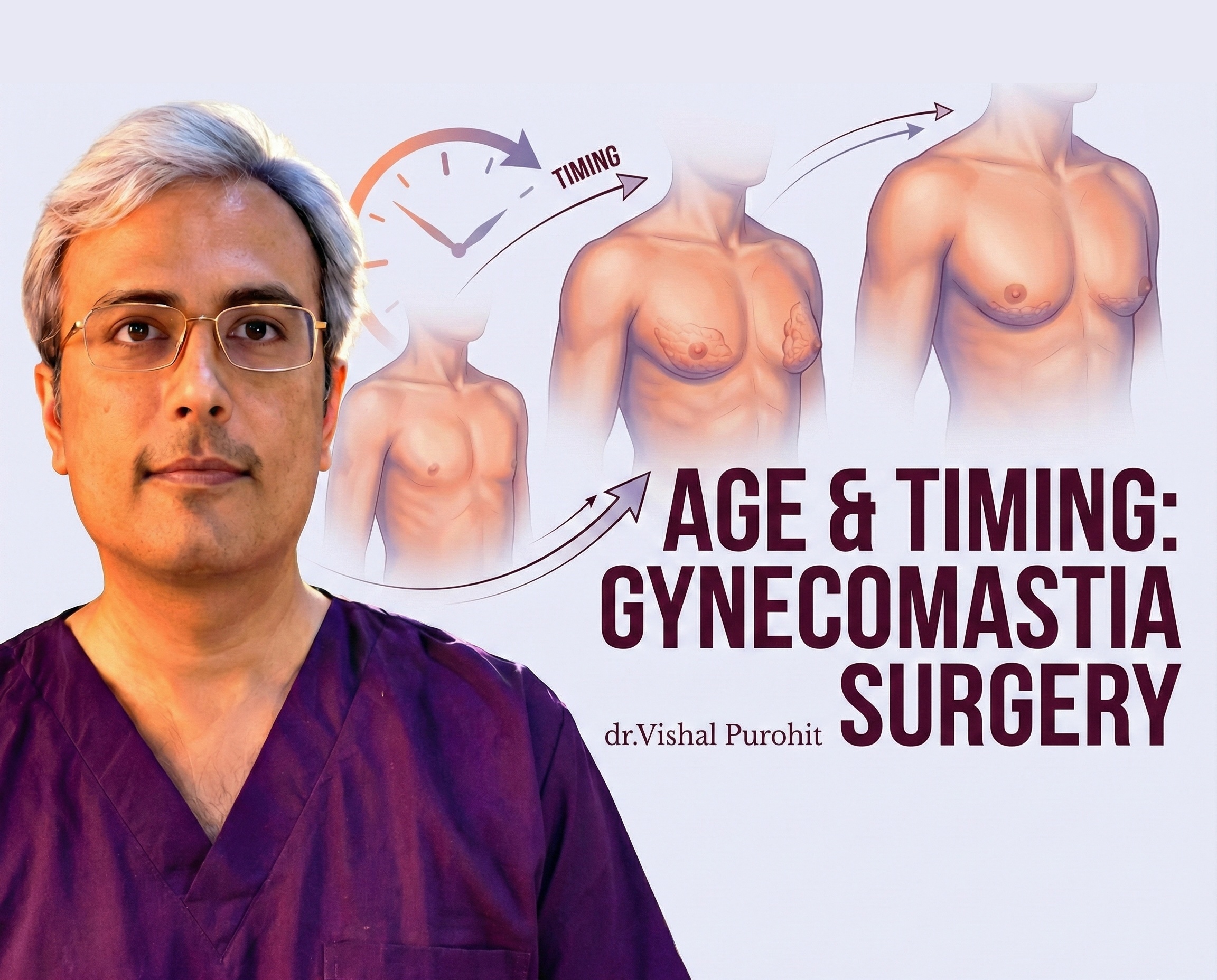
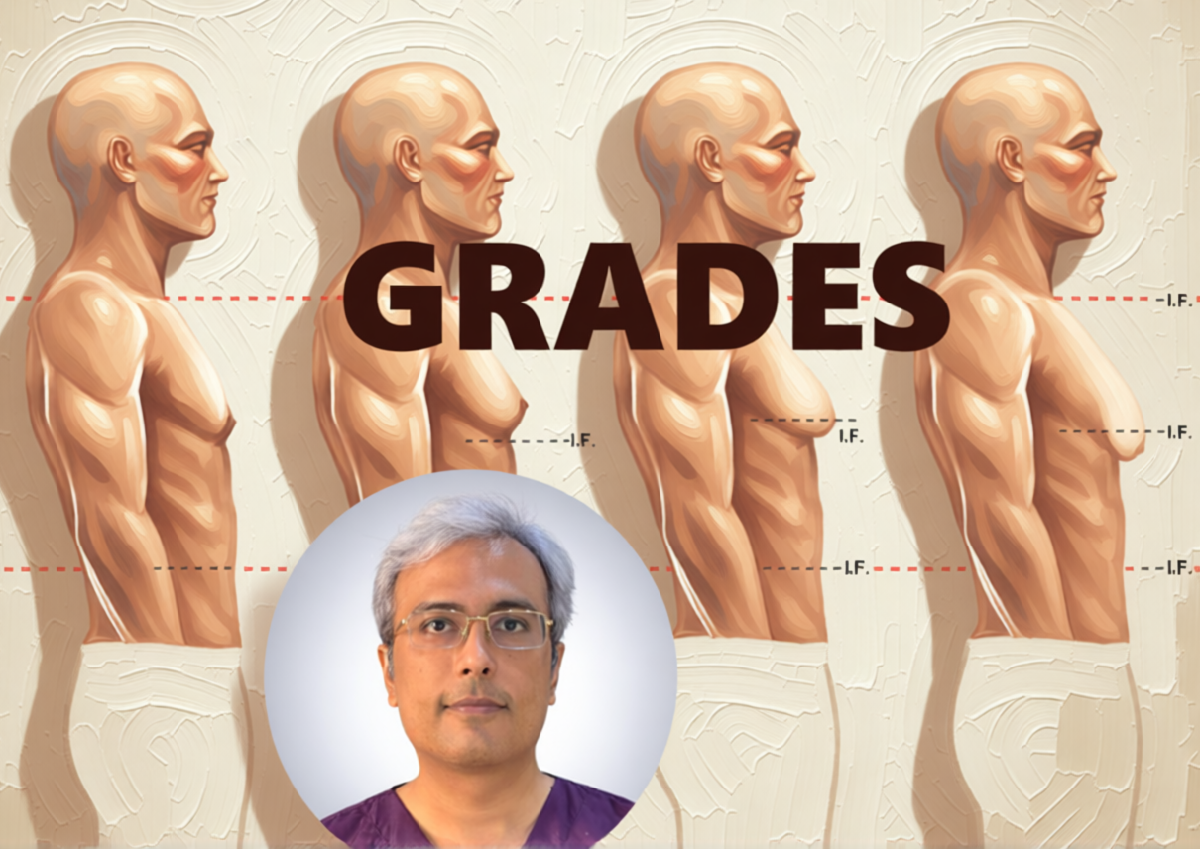
The extent of scarring depends heavily on the severity of your condition. We use the Simon Classification system to grade the severity, which helps us predict the necessary incision length.
- Grade 1 & 2 (Minor to Moderate): These usually require only the hidden periareolar incision. The risk of visible scarring is extremely low.
- Grade 3 (Significant Enlargement): Still typically managed with the standard hidden incision.
- Grade 4 (Excess Skin): In severe cases, particularly after massive weight loss, the skin may not retract on its own.
- The Trade-Off: In these cases, we may need to remove excess skin. Research indicates that while this approach may leave more scars, it results in a flatter chest wall, which is often the patient’s priority over a slight scar. However, most standard cases do not require this.
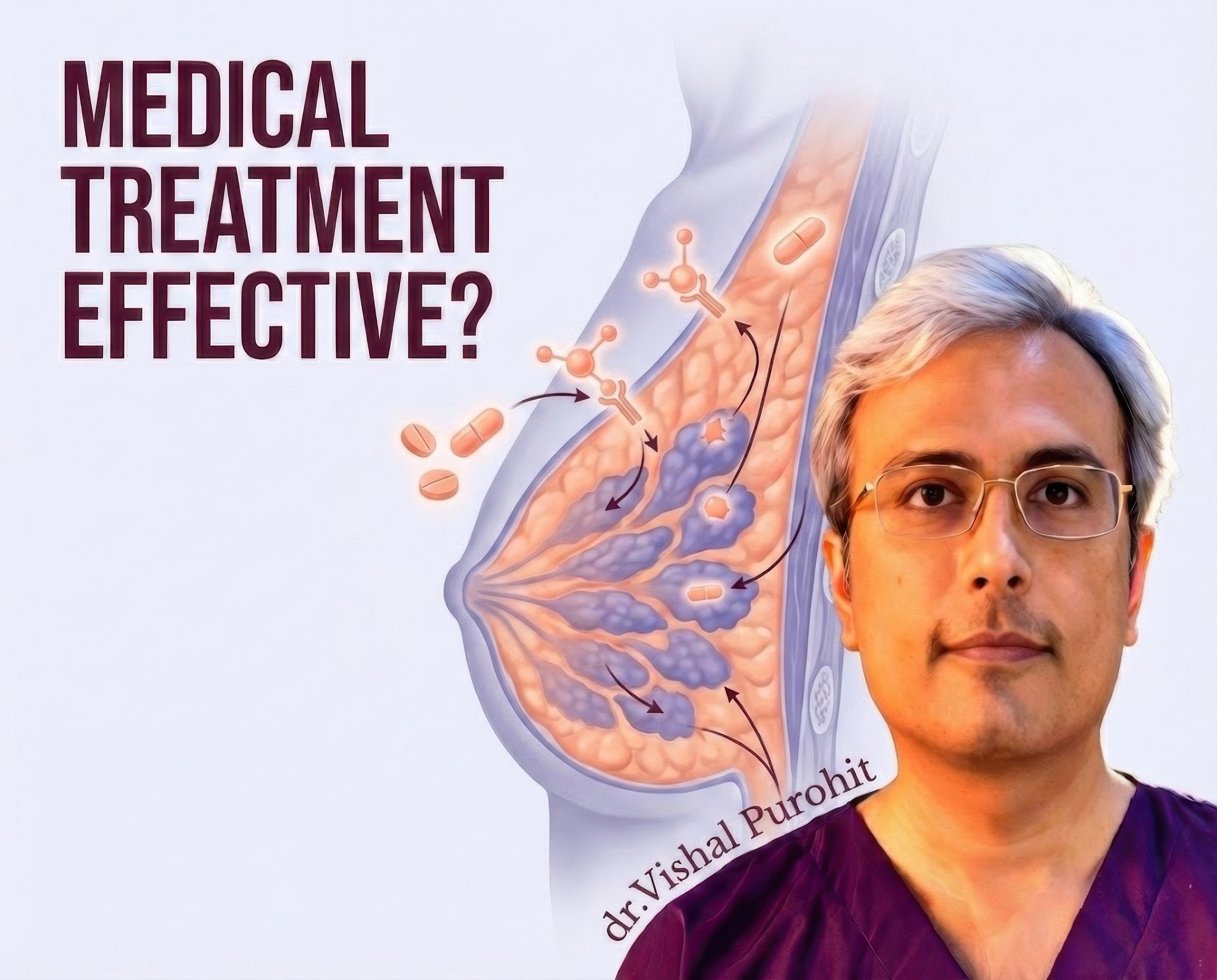
Why Not Just Liposuction? (Avoiding Bad Scars)
Some patients ask for “liposuction only” to avoid the small nipple scar. However, this can backfire.
If the gland is not removed, you may be left with a concave or uneven chest. Studies show that surgical excision of the gland is often required to prevent residual deformity.
Furthermore, trying to remove a hard gland through a tiny liposuction hole can traumatise the skin, leading to worse scarring or residual gynecomastia that requires a second surgery. A clean, precise incision heals far better than traumatised skin.
Post-Op Protocol: How to Minimise Scarring
Great surgery is 50% of the result; how you heal is the other 50%. Following our Gynecomastia Recovery Guide is essential, but here are specific tips for your scars:
- Sun Protection (Critical): Fresh scars turn dark (hyperpigmentation) if exposed to UV rays. You must keep your chest covered or use high-SPF sunscreen for the first 6 months.
- Silicone Gel Sheets: We often recommend medical-grade silicone gel. Evidence suggests it helps flatten and fade scars by keeping the tissue hydrated.
- Massage: Once the incision is fully closed (usually after 3 weeks), gentle massage helps break down internal scar tissue and softens the area. (Remember only message the scar, not the chest)
Frequently Asked Questions
Where are the scars located after gynecomastia surgery, and how visible are they?
The most common location for the incision is the semicircular intra-areolar incision, positioned along the inferior margin of the areola to ensure the resulting scar is well-camouflaged by the natural pigment transition. In cases involving significant skin redundancy, the incisions may need to extend around the full circumference of the areola or onto the chest wall, though surgeons strive to keep these within aesthetic boundaries to limit visibility.
In modern minimally invasive approaches, the operation can often be performed through a single puncture incision located on the lateral chest wall or within the axilla (armpit), which heals as a barely noticeable mark. This approach is favoured because it avoids placing any cuts directly on the front of the breast mound, keeping the chest wall pristine.
For the vast majority of patients with mild to moderate gynecomastia, the goal is to place incisions where they are least likely to be seen. This results in what many patients describe as an inconspicuous scar that does not draw unwanted attention to the chest.
However, in severe cases requiring skin resection, longer scars may be necessary. Even in these instances, techniques are employed to hide these scars in natural folds or along the border of the areola, ensuring they remain as discreet as possible once healed.
How long does it take for gynecomastia surgery scars to fade?
Immediately following surgery, incisions will naturally appear red and slightly raised, but this is a normal part of the inflammatory healing process that improves significantly over time. In many cases, even fine suture tracks or incision lines become unnoticeable at 3 months post-operatively as the tissue remodels.
The complete maturation of the scar can take longer, and patience is required. For example, it has been observed that scars may remain hyperchromic (darker) for about 2 months before returning to a normal skin colour around 8 to 9 weeks.
While the fading process varies by individual skin type and pigmentation, the majority of scars settle into thin, white lines that blend well with the surrounding skin within 3 to 12 months.
During this maturation phase, the scar goes through remodelling, where collagen is broken down and replaced. Ultimately, for most patients, the final scar is barely perceptible and is considered a worthwhile trade-off for the improved chest contour.
What can I do to minimise scarring after my gynecomastia procedure?
To minimize scarring, it is crucial to employ surgical techniques that reduce tension on the wound edges, such as using external quilting sutures to obliterate dead space and prevent hematomas, which can lead to poor wound healing and abnormal scars.
Post-operatively, adhering strictly to the surgeon’s instructions regarding the use of compression garments is vital. These garments help control swelling and support the skin as it retracts, thereby reducing the risk of scar widening or hypertrophy.
Choosing a surgeon who uses minimally invasive approaches, such as the cartilage shaver or pull-through technique, also plays a major role by allowing significant glandular removal through tiny incisions that inherently heal with less scarring.
Finally, avoiding activities that stretch the incision site prematurely is important, particularly in the first few weeks. Excessive movement or strain on the healing wound can cause scar widening, so restricting arm movements as advised is a key step in scar management.
Are gynecomastia surgery scars permanent, or can they be removed or improved later?
While surgical scars are technically permanent, their visibility can be significantly improved if they heal poorly or become hypertrophic (raised and red). In cases where scars become raised or thickened, non-surgical treatments such as local steroid injections have been shown to effectively flatten and soften the scar tissue.
If a scar is particularly unsightly, wide, or tethered, surgical revision can be performed. This is often a minor procedure done under local anaesthesia to excise the old scar and re-close the wound more precisely, a strategy often reserved for grade IV gynecomastia cases where initial tension may have been high.
It is worth noting that patient perception plays a role in how “permanent” a scar feels. Some patients view these scars as a positive trade-off, a “mark of distinction” compared to the negative stigmata of breast enlargement, meaning they are rarely bothered enough to seek removal.
Ultimately, while the mark remains, its impact on your appearance can be managed. With proper care and time, most scars fade to the point where they are not a source of concern.
Do different surgical techniques lead to different types of scars in gynecomastia treatment?
Yes, the choice of surgical technique directly dictates the type and extent of scarring. Traditional extensive excisions can leave long, noticeable scars across the chest, which is why modern practice has shifted toward less invasive methods.
Techniques like the pull-through method allow for the removal of glandular tissue through a tiny incision, resulting in a scar that is barely perceptible after maturation. This contrasts sharply with open techniques required for severe cases.
When treating severe gynecomastia (Grade III or IV) with significant skin excess, skin resection is often required, which inevitably leads to longer scars, potentially around the areola or extending horizontally on the chest.
However, advancements like the endoscopic subcutaneous mastectomy allow for gland removal via an axillary incision, leaving the anterior chest wall completely free of scars, demonstrating how technique selection is the primary factor in scar outcome.
Invest in Skill, Not Just Surgery
The visibility of a scar is heavily dependent on the surgeon’s suturing technique. Dr. Vishal Purohit uses multi-layered closure techniques to ensure there is no tension on the wound, resulting in the finest possible line.
If you are worried about the aesthetic outcome, don’t guess. Come in for a consultation and see our “Before & After” gallery to judge the results for yourself.
- 📞 Call/WhatsApp: +91 7718183535
- 📍 Visit Us: Kalpana Aesthetics, Jaipur
- 📅 Book Your Consultation
Disclaimer: The content provided in this blog post is for informational and educational purposes only and does not constitute medical advice. Individual healing rates and scar formation can vary based on genetics. Always consult with a board-certified plastic surgeon.