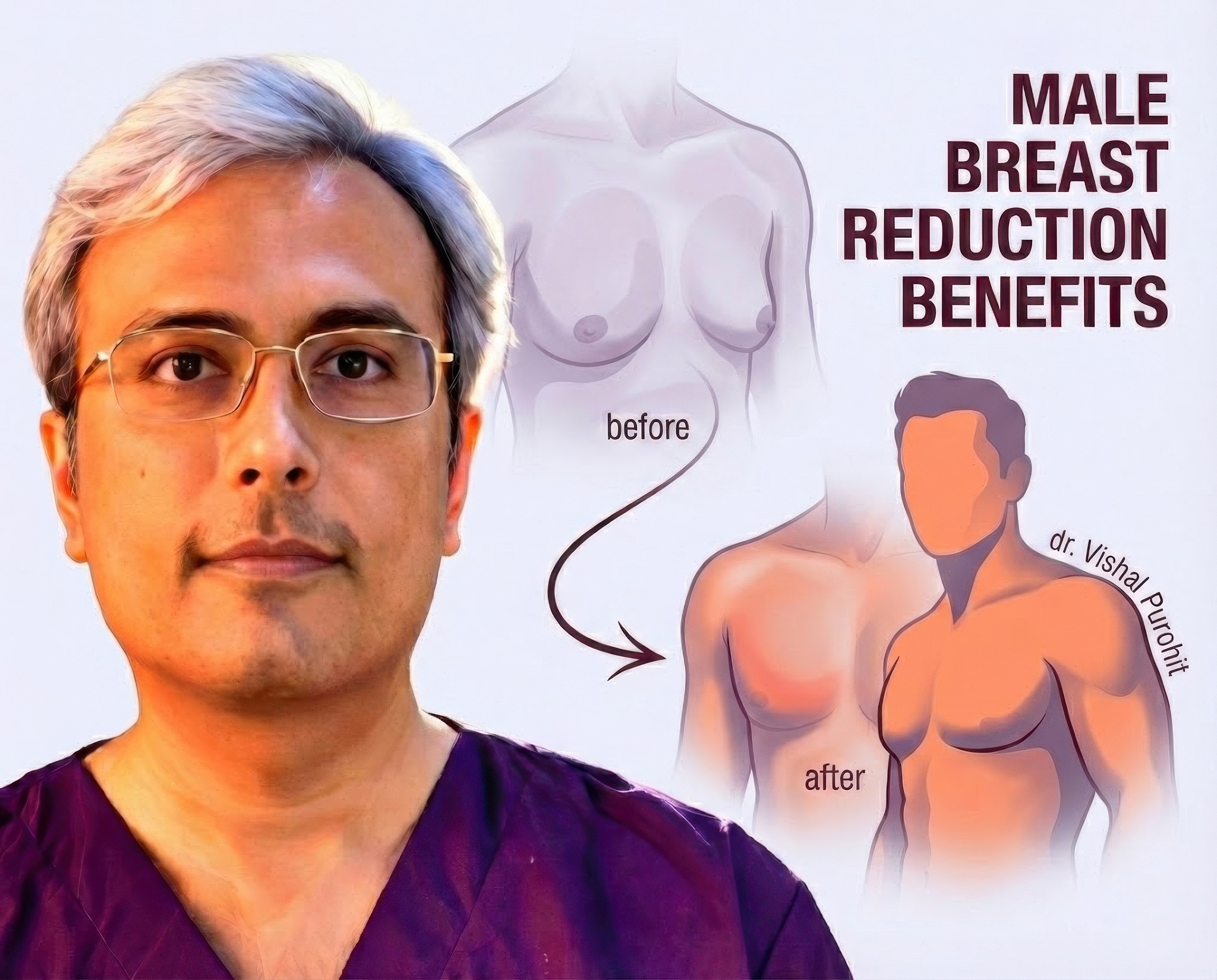
The decision to move forward with gynecomastia treatment is a fantastic step toward renewed confidence. However, a safe and successful procedure is built on a foundation of meticulous preparation.
Many patients ask, “Am I an ideal candidate?” or “What tests do I need?”
This guide outlines the mandatory steps of your journey with Dr Vishal Purohit, ensuring that you are physically and mentally ready for your transformation.
Phase 1: Am I an Ideal Candidate for Gynecomastia Surgery? (Eligibility)
Before we schedule any procedure, we must first establish eligibility. Not everyone with a larger chest needs surgery, and not everyone is ready for it immediately.
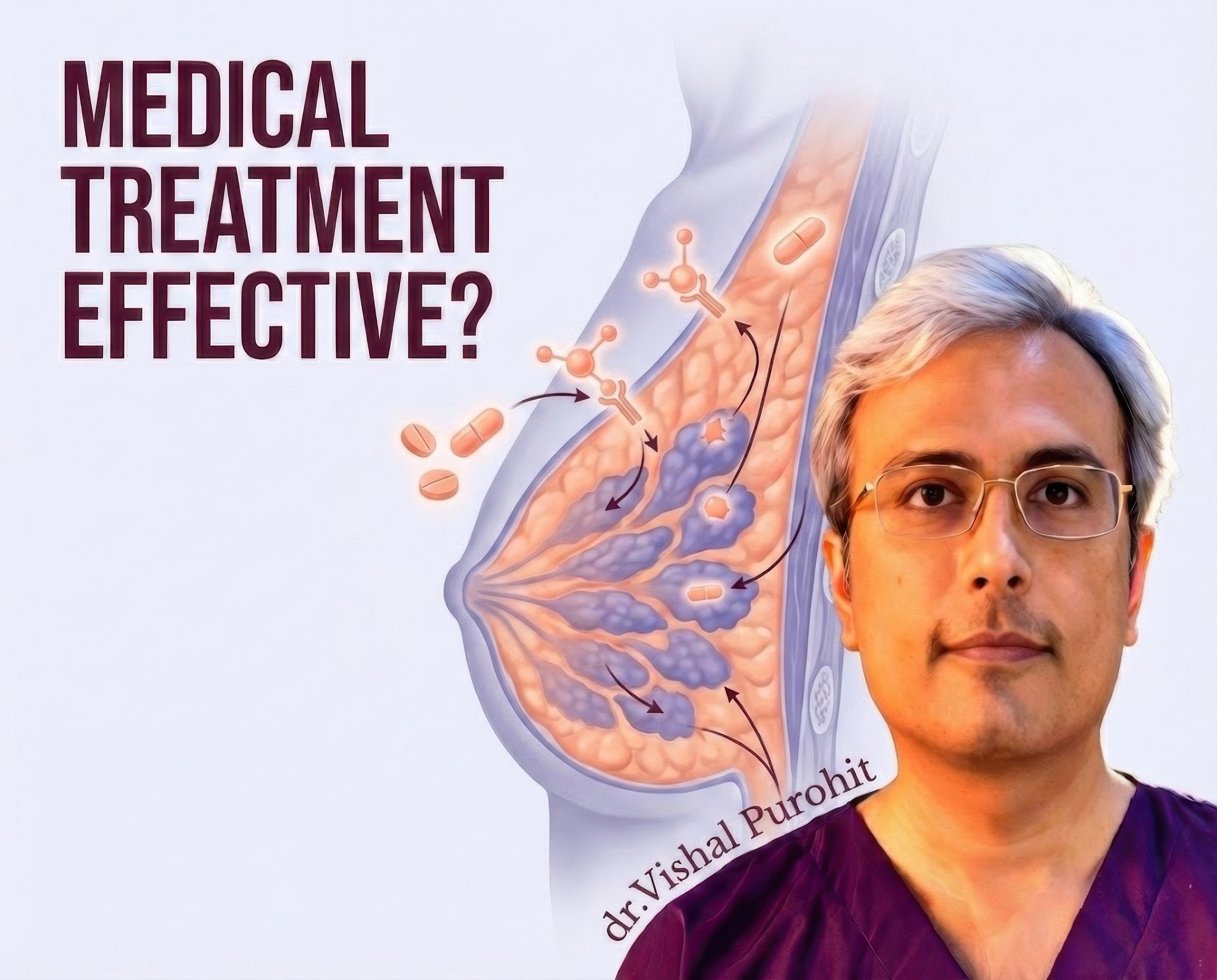
If your condition is in the very early, painful stage, we may first explore medical treatment options for gynecomastia to see if the gland size can be reduced without surgery.
The “True Gynecomastia” Test
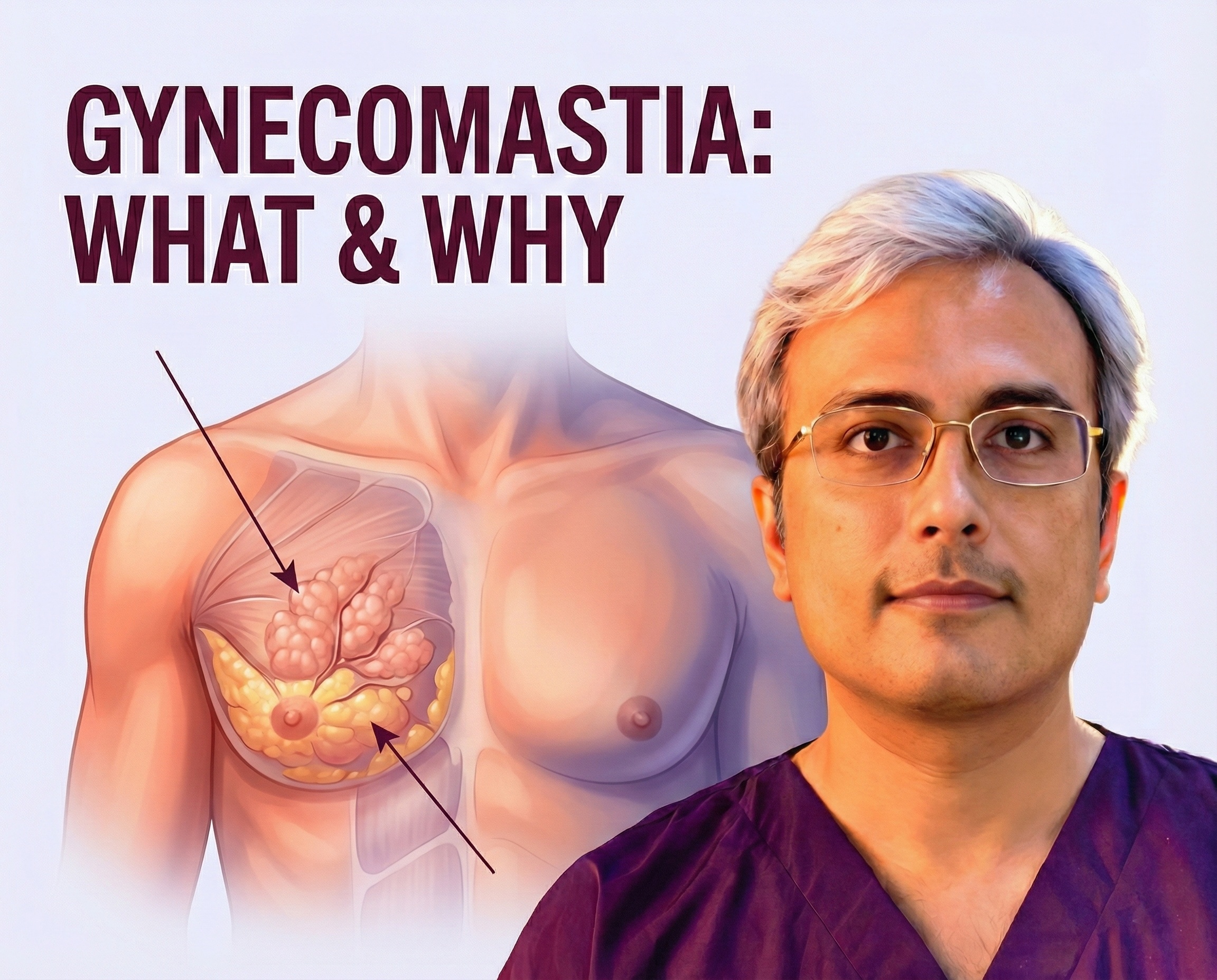
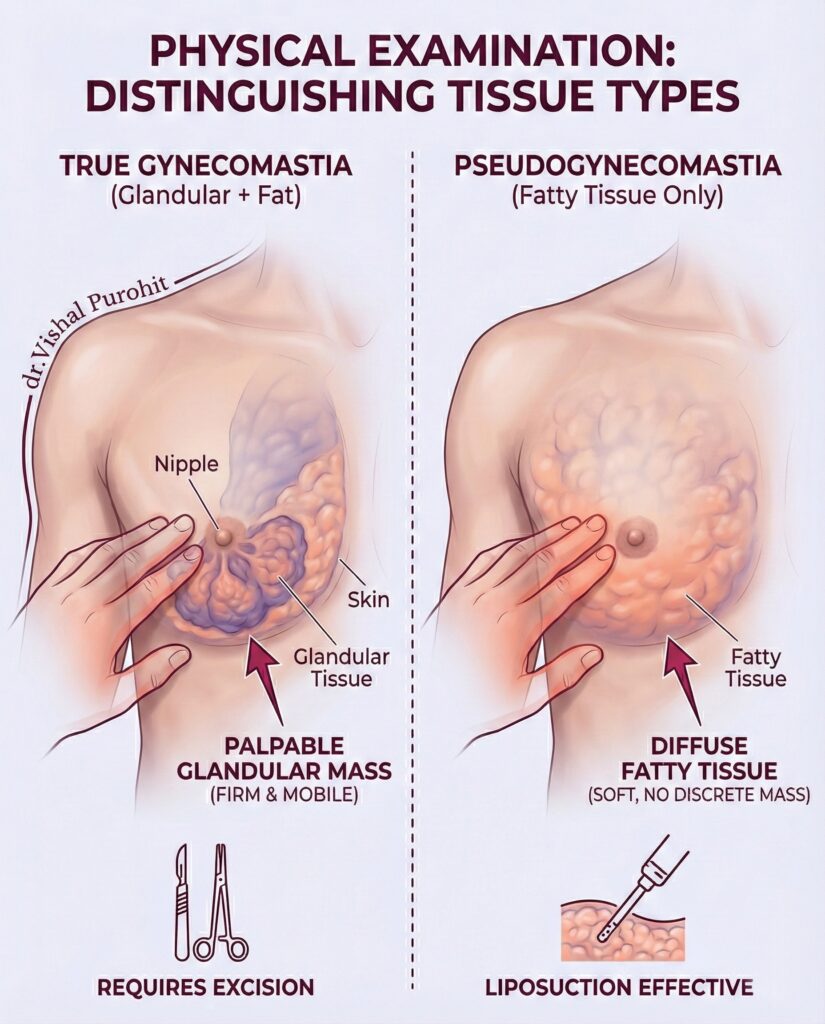
The most critical factor is diagnosing True Gynecomastia (glandular tissue) versus Pseudo-Gynecomastia (excess fat).
- Pseudo-Gynecomastia: Often resolves with diet and exercise.
- True Gynecomastia: Involves firm, rubbery glandular tissue that cannot be exercised away. Medical literature confirms that for established glandular tissue, surgical excision remains the gold standard for effective correction. Learn more about the condition in our Gynecomastia Definition Guide.
Health & Lifestyle Check
To be an ideal candidate, you should be:
- Medically Healthy: No uncontrolled chronic conditions (like diabetes or bleeding disorders).
- Stable Weight: You should be near your ideal body weight. Significant weight fluctuations after surgery can alter your results.
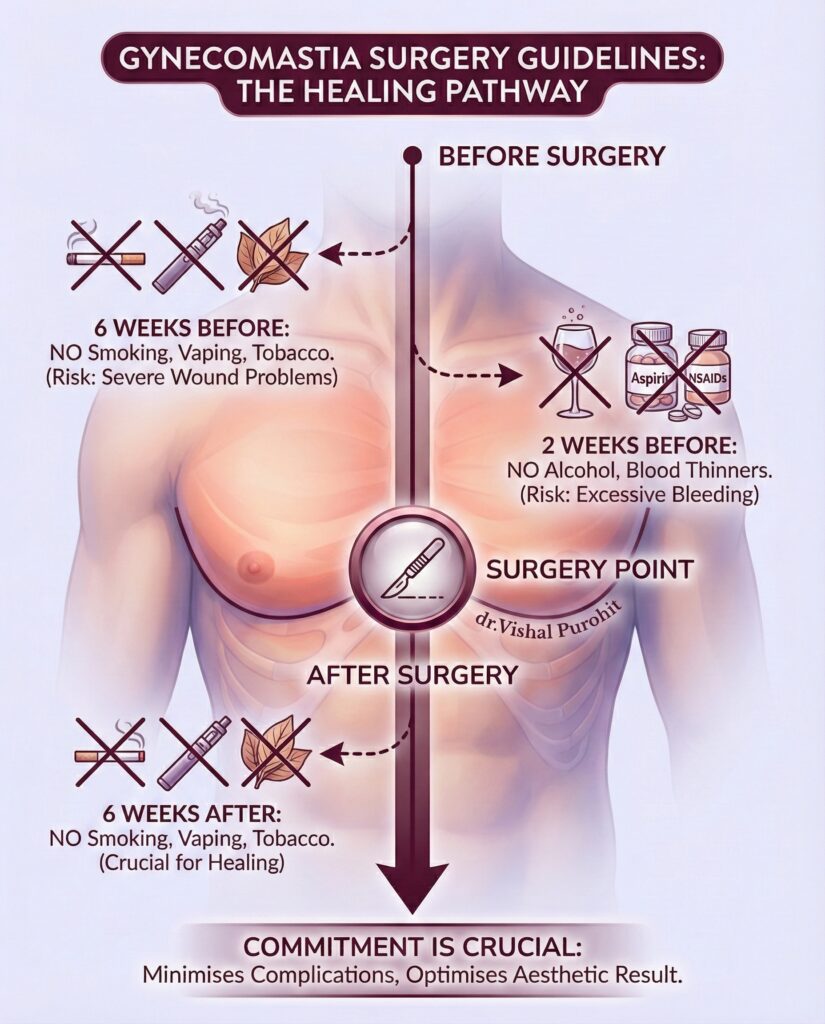
- Non-Smoker: Smoking severely constricts blood vessels and impedes healing. You must be willing to stop smoking for at least 3 weeks before and after surgery.
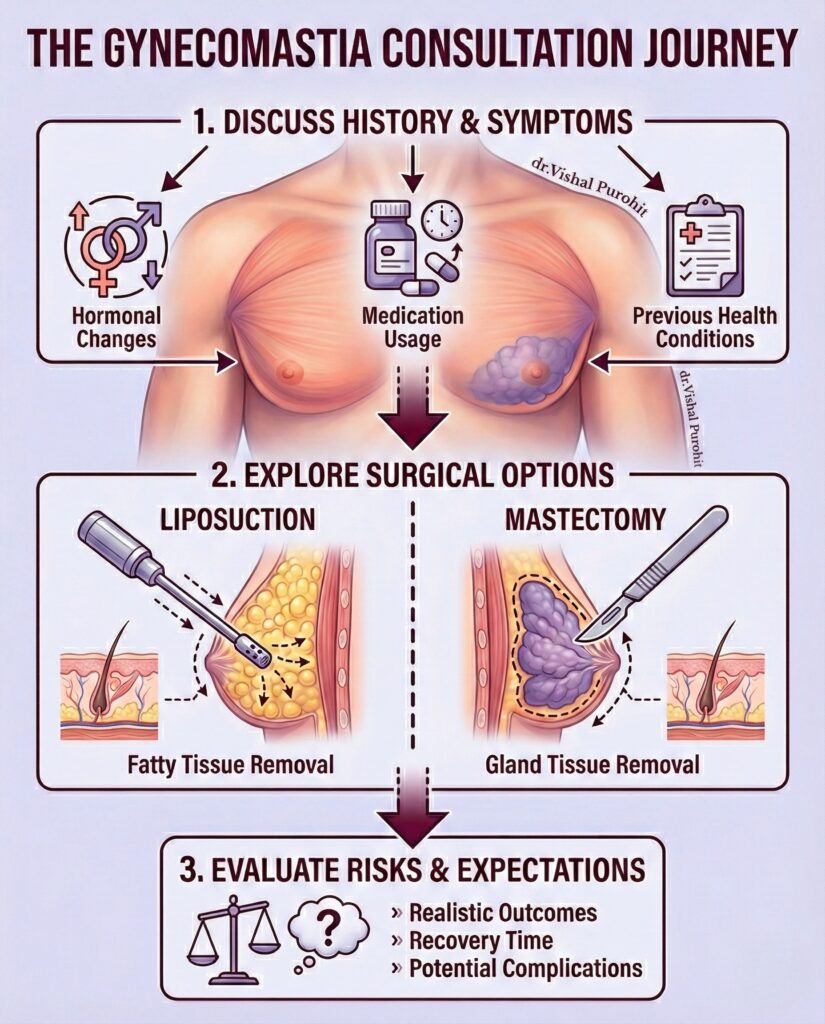
Phase 2: The Consultation
The consultation is not just a chat; it is a comprehensive clinical evaluation before planning gynecomastia surgery. This is where we create your customised surgical plan.
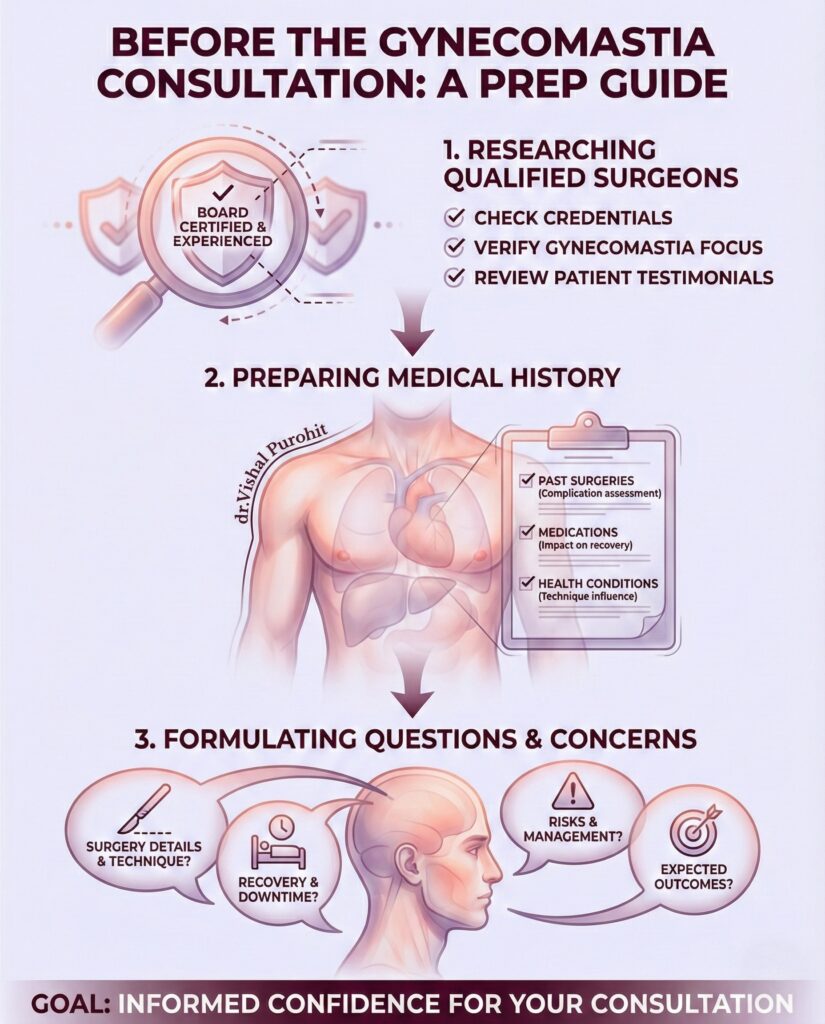
What Happens During the Consultation for Gynecomastia Surgery?
- Physical Examination: Dr. Vishal Purohit will palpate the chest to determine the ratio of fat to gland. This dictates whether you need Liposuction, Gland Excision, or both. Read about the Gynecomastia Surgery Techniques here.
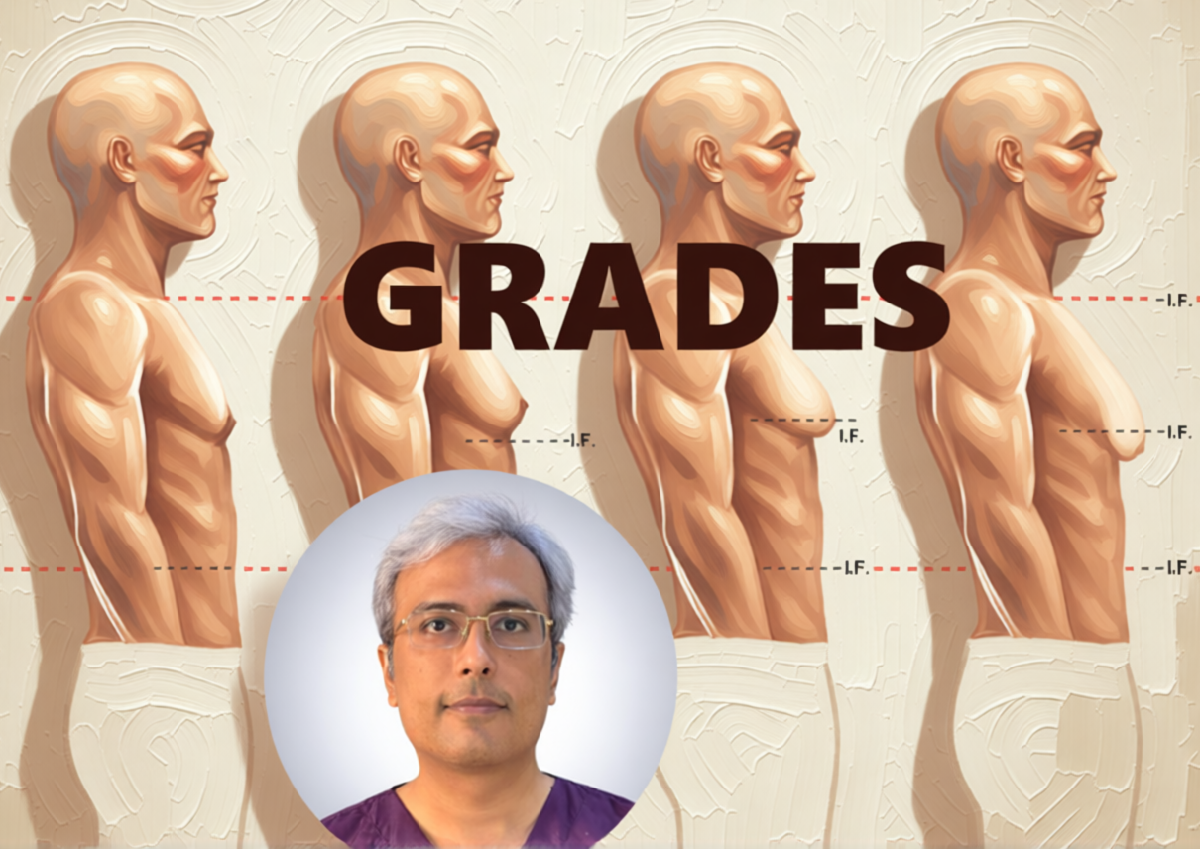
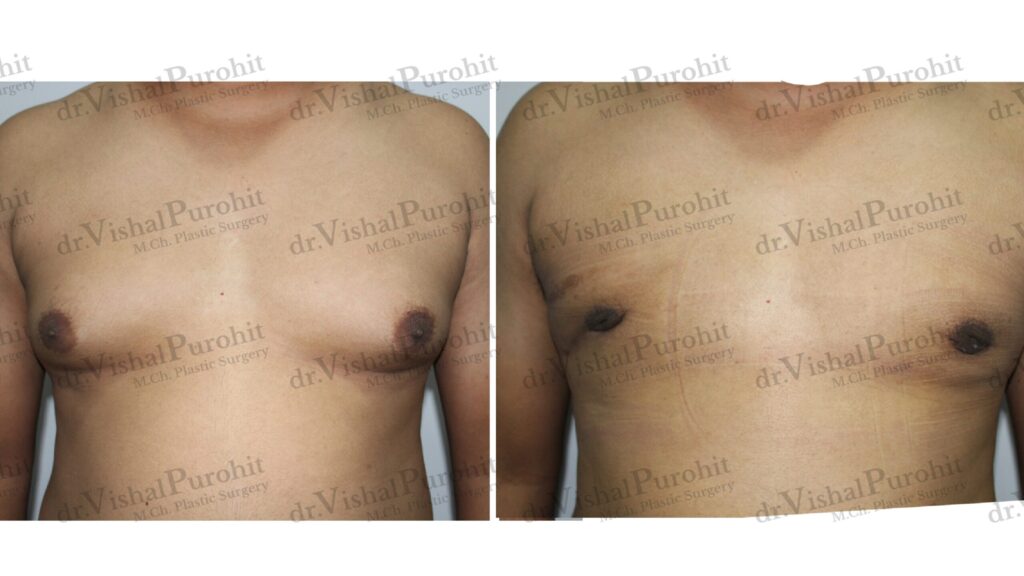
- Grading: We will classify your condition (Grade 1 to 4) to determine the complexity and Cost of the gynecomastia procedure.
- Medical History Review: We will review any medications you are taking (e.g., steroids, hair loss medication) that might have caused the condition.
Phase 3: Mandatory Diagnostic Tests (Screening)
Gynecomastia can sometimes be a symptom of underlying health issues. Therefore, comprehensive lab testing is mandatory before we proceed. We do not operate without these safety clearances.
During the consultation, we will determine the grade of gynecomastia you have, which dictates the surgical approach.
Essential Tests
- Hormonal Assay: To ensure your hormone levels (Testosterone, Estrogen, Prolactin, Thyroid) are stable. If an active hormonal imbalance exists, it must be treated by an endocrinologist first to prevent regrowth.
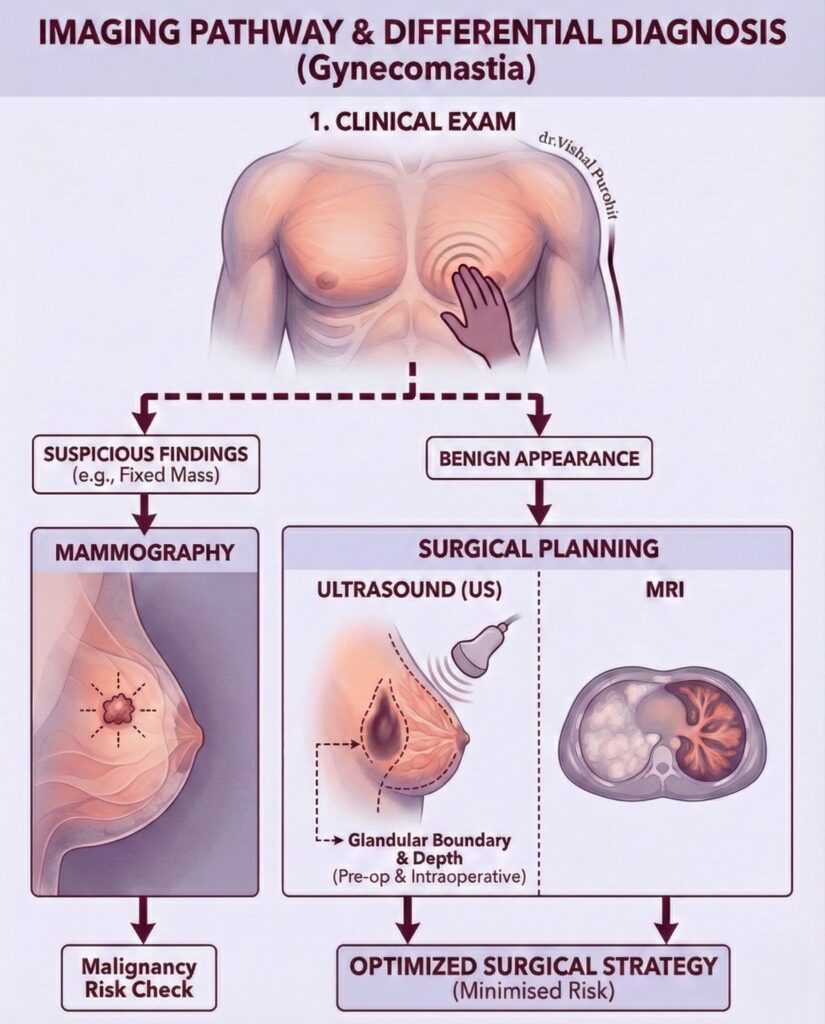
- Ultrasound / Mammography: To confirm the presence of benign glandular tissue and rule out rare male breast cancer.
- Routine Pre-Op Panel: CBC (Complete Blood Count), LFT (Liver Function Test), KFT (Kidney Function Test), and coagulation profile to ensure you are safe for anaesthesia.
Research Note:
Thorough preoperative evaluation is critical. Clinical guidelines emphasize that identifying secondary causes (such as tumors or endocrine disorders) via diagnostic screening is vital before surgical correction to ensure patient safety.
Phase 4: The “Readiness” Checklist (2 Weeks Before)
Once your tests are cleared and your surgery is booked, you enter the “Readiness” phase. Following these steps is not optional; it is critical for a smooth recovery.
Medications to Stop
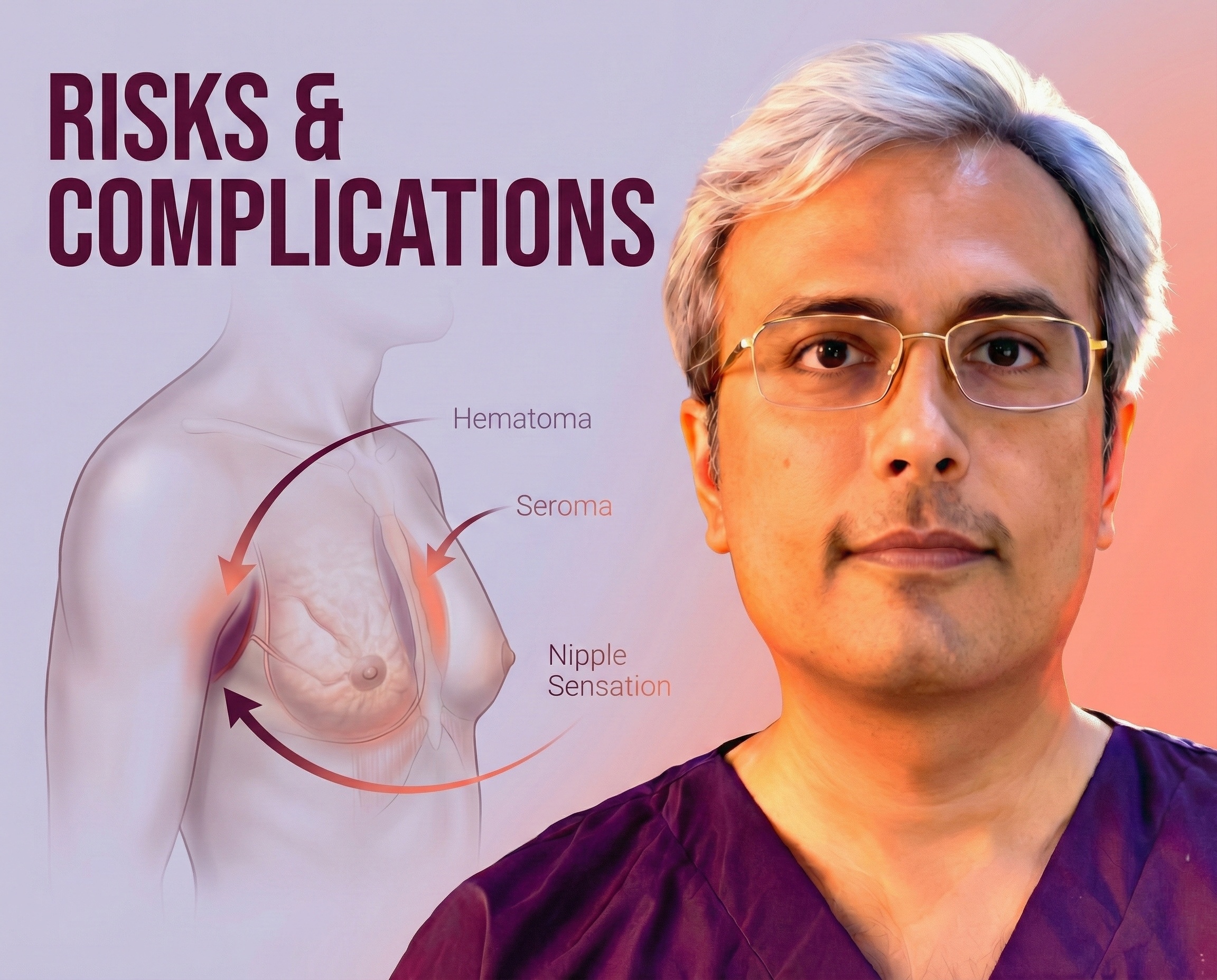
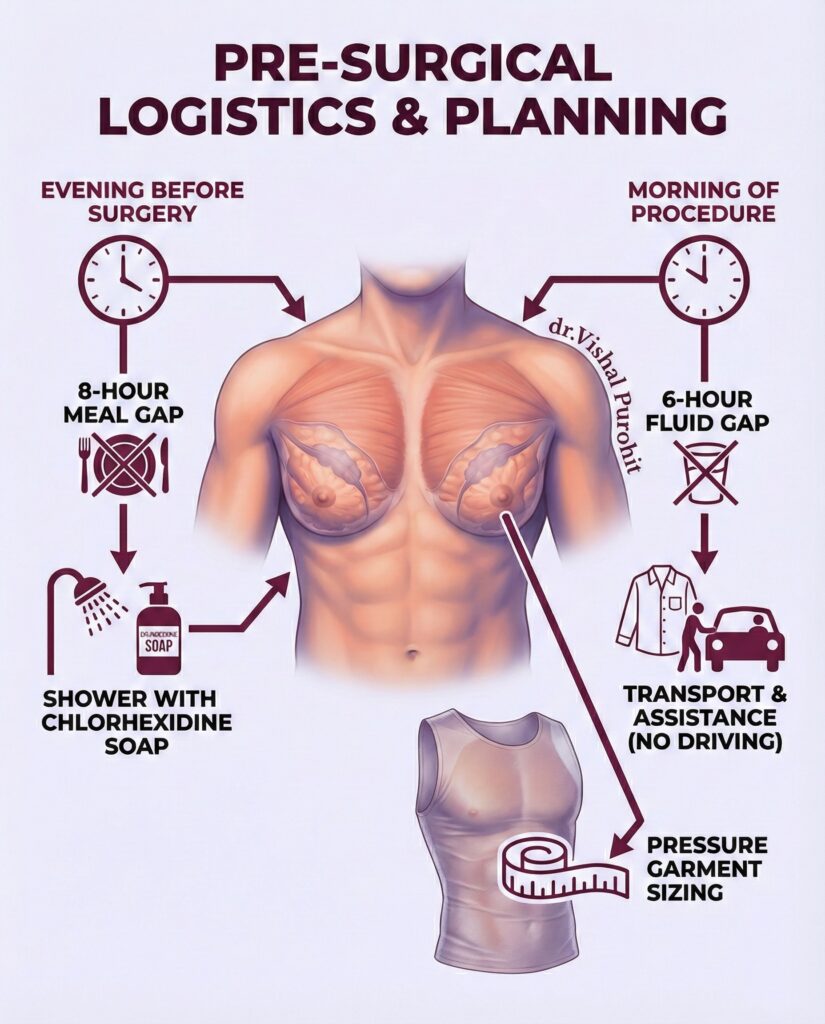
- Blood Thinners: Stop taking Aspirin, Ibuprofen, or Vitamin E supplements at least 10 days prior to surgery to reduce the risk of bleeding (hematoma).
- Supplements: Avoid herbal supplements (like Ginkgo Biloba or Ginseng) as they can interfere with anesthesia.
Lifestyle Adjustments
- Hydration: Drink 3-4 litres of water daily to keep your skin hydrated and elastic.
- Arrangements: Organise a friend or family member to drive you home after the surgery. You cannot drive while under the influence of anaesthesia.
- Clothing: Buy comfortable, button-down shirts. You will not be able to lift your arms overhead to put on a t-shirt for the first few days.
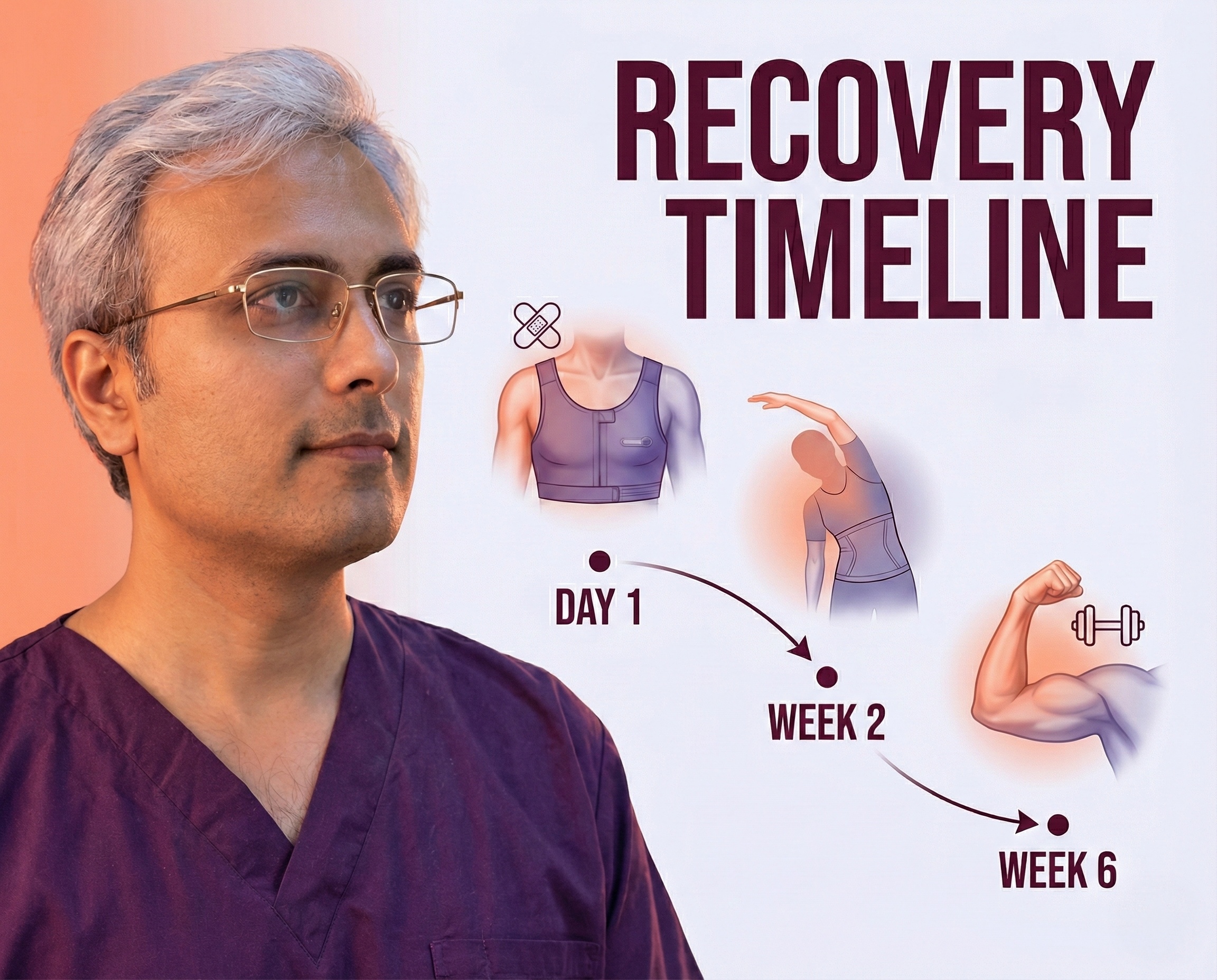
Worried about the days following surgery? Review our full Gynecomastia Surgery Recovery Timeline Guide.
Frequently Asked Questions
What are the eligibility criteria for gynecomastia surgery?
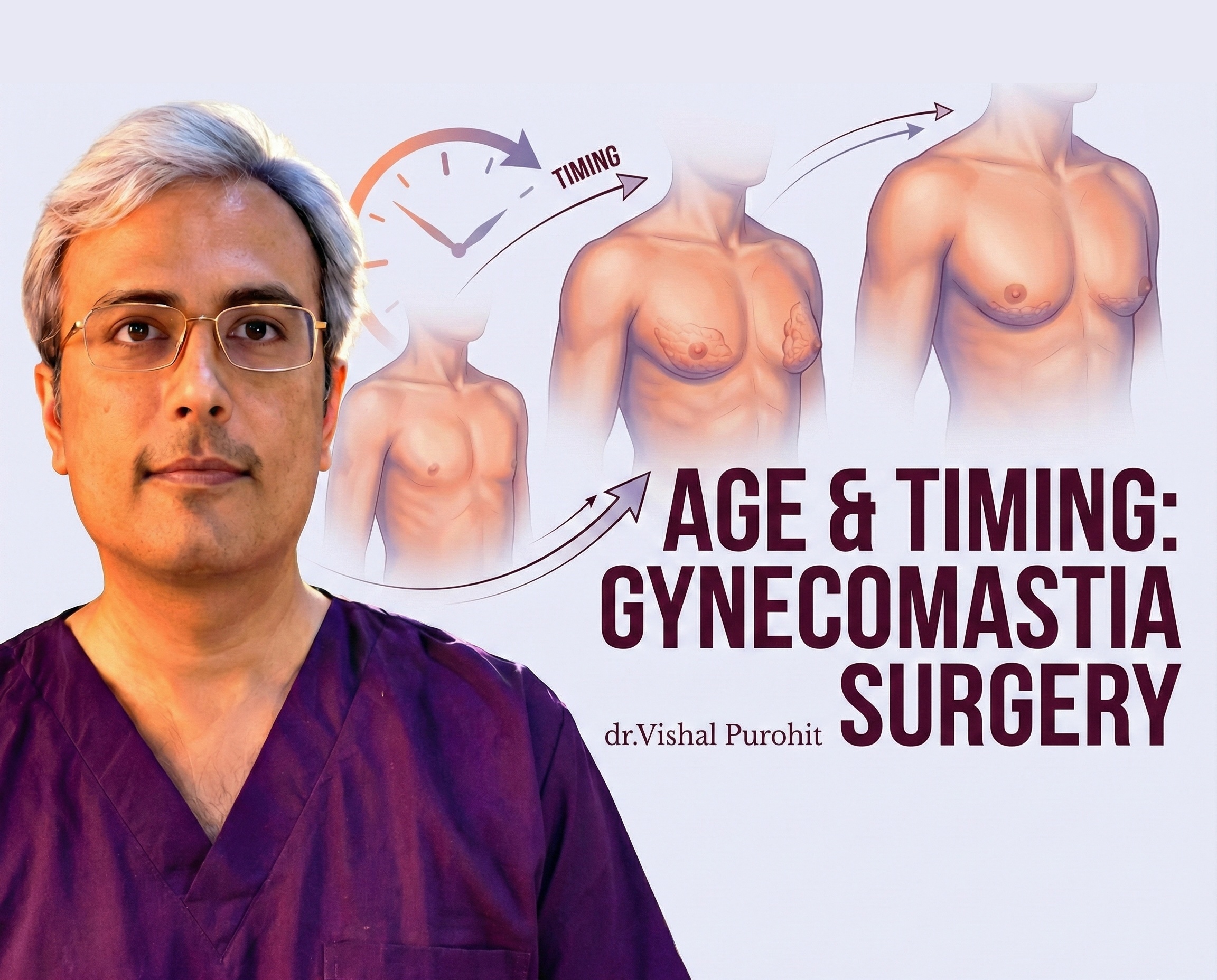
Eligibility for gynecomastia surgery is primarily determined by the persistence and nature of the breast enlargement. Generally, candidates are those whose condition has stabilised and failed to regress spontaneously or respond to medical therapy. For adolescents, surgery is often considered only if the condition has persisted for more than two years or causes significant psychosocial distress, as many cases in this age group resolve on their own. In adults, surgery is indicated if the hypertrophic breast tissue has been present for more than 12 months, as fibrosis likely renders the tissue irreversible to non-surgical treatments.
The presence of physical symptoms is another key criterion for eligibility. Patients often seek surgical intervention due to pain, tenderness, or physical discomfort associated with the breast enlargement. Beyond physical symptoms, the psychological impact is a major factor; eligibility is strongly supported when the patient experiences significant emotional distress, embarrassment, or a diminution of his self-esteem due to the appearance of his chest. This psychosocial burden often interferes with daily activities and social interactions, justifying the need for correction.
Furthermore, patients must be screened to ensure the gynecomastia is not secondary to an active, treatable underlying condition. Before proceeding with surgery, it is essential to rule out causes such as drug use, anabolic steroids, or treatable endocrine disorders. If the gynecomastia is drug-induced, the offending agent should be discontinued for several months to observe if regression occurs before surgery is considered. Eligible candidates are typically those with idiopathic gynecomastia or those whose primary cause has been addressed, but the breast tissue remains.
Finally, the physical characteristics of the breast tissue play a role in eligibility and surgical planning. Patients are assessed based on the grade of gynecomastia, which ranges from minor enlargement to severe hypertrophy with skin redundancy. Candidates with significant skin excess may require more complex procedures involving skin resection. Overall, the ideal candidate is a healthy male with a persistent benign enlargement of the breast that has been stable and is a source of physical or mental hardship.
What medical evaluations and tests are required before gynecomastia surgery?
A comprehensive medical evaluation begins with a detailed history and physical examination to distinguish true gynecomastia from pseudogynecomastia and to identify potential underlying causes. The physical exam focuses on assessing the breast tissue consistency, checking for palpable breast nodules, and looking for signs of malignancy such as fixation or nipple discharge. The examination also includes a genital assessment to check for testicular masses or atrophy, which could indicate a hormonal imbalance or tumour.
Laboratory testing is a standard requirement to rule out systemic or endocrine disorders. A routine panel typically includes renal and liver function tests, as dysfunction in these organs can alter hormone metabolism. Specific hormonal assays are also conducted, including measurements of serum testosterone, estradiol, luteinizing hormone (LH), follicle-stimulating hormone (FSH), prolactin, and human chorionic gonadotropin (hCG),. These tests help exclude conditions such as hypogonadism, hyperthyroidism, or hormone-secreting tumours.
Imaging studies are essential for characterising the breast tissue and ruling out malignancy. A breast ultrasound is often the primary modality used to confirm the presence of glandular tissue versus fatty tissue and to classify the gynecomastia severity. In older patients or those with suspicious clinical findings, mammography may be utilised to ensure there is no evidence of breast cancer. Additionally, a testicular ultrasound might be ordered if there are abnormalities in the genital exam or hormonal profile.
In some cases, further specific testing may be warranted based on clinical findings. For instance, if there is a suspicion of a genetic disorder like Klinefelter syndrome, a chromosomal analysis (karyotype) may be performed. Fine-needle aspiration cytology (FNAC) or core biopsy is generally reserved for cases where imaging or physical examination suggests a potential malignancy, rather than for routine diagnosis of gynecomastia. This thorough workup ensures that surgery is appropriate and safe for the patient.
How should I prepare physically and lifestyle-wise before undergoing gynecomastia surgery?
Physical preparation often involves optimising body weight and composition. Weight loss is frequently recommended as a first-line step, especially for patients who are overweight or obese, to help distinguish between true glandular gynecomastia and pseudogynecomastia, which is primarily fatty tissue. Reducing body fat can minimise the extent of surgery required and improve the final aesthetic contour of the chest. However, patients should be aware that glandular tissue will not regress with weight loss alone.
Lifestyle modifications regarding substance use are critical for surgical safety and healing. Patients are strongly advised to stop smoking for a significant period before and after the procedure, as smoking can impair wound healing and increase the risk of complications like necrosis. Specifically, nicotine abstinence is often required for at least two weeks prior to surgery and three weeks post-operatively. Furthermore, patients should discontinue the use of any recreational drugs, such as marijuana or anabolic steroids, which may have contributed to the condition.
Medication management is another essential aspect of preparation. Patients are typically instructed to stop taking aspirin, ibuprofen, vitamin E, and other blood-thinning supplements for at least 10 days before surgery to reduce the risk of intraoperative bleeding and postoperative haematoma formation. It is important to disclose all medications and supplements to the surgeon to ensure they do not interfere with anaesthesia or coagulation.
Finally, patients should prepare mentally and logistically for the recovery period. This includes arranging for time off work or school and organising help for the first few days after surgery. Understanding that there may be temporary activity restrictions, such as avoiding strenuous exercise, is part of the preparation. In some cases, specific dietary adjustments or supplements may be suggested to support healing, particularly for patients with nutritional deficiencies or those who have undergone massive weight loss.
Are there age or health conditions that affect whether someone can have gynecomastia surgery?
Age is a significant factor in determining eligibility for gynecomastia surgery. In adolescents, surgery is generally postponed until puberty has stabilised, as the condition often regresses spontaneously within 1 to 2 years. Surgical intervention in this age group is typically reserved for cases that have persisted for more than two to three years or cause severe psychological distress. Conversely, in elderly men, gynecomastia is often secondary to declining testosterone levels or medication, and the surgical risk profile must be weighed against comorbidities.
Obesity is a major health condition that impacts surgical candidacy. Patients with a body mass index (BMI) greater than 25 kg/m2 or those classified as morbidly obese are at a significantly higher risk for postoperative complications, such as wound healing problems and haematomas. Consequently, many surgeons may require weight loss prior to surgery or may consider obesity a relative contraindication until a lower BMI is achieved.
Systemic health conditions can also affect eligibility. Underlying causes such as chronic renal failure, liver cirrhosis, or hyperthyroidism must be managed before considering cosmetic correction. If the gynecomastia is secondary to these conditions, treating the primary disease may resolve the breast enlargement without the need for surgery. Additionally, severe cardiovascular or respiratory conditions may make elective surgery unsafe.
The presence of malignancy is a critical exclusion criterion for standard gynecomastia surgery. Although rare, male breast cancer must be ruled out, especially in older patients or those with unilateral, hard masses. If a testicular tumour or other neoplasm is identified as the cause of estrogen excess, the priority shifts to oncological treatment rather than aesthetic correction of the breast.
What questions should I ask my surgeon during the pre-surgery consultation?
During the consultation, it is crucial to ask about the specific surgical technique the surgeon plans to use. You should inquire whether they will use conventional liposuction, ultrasound-assisted liposuction, or direct excision, and why they recommend that specific approach for your anatomy. Understanding the technique helps manage expectations regarding the extent of the procedure and the likely results.
You should also ask about the potential risks and complications associated with the surgery. Specifically, inquire about the risk of postoperative hematoma or seroma, and whether the surgeon uses drains to mitigate these risks. It is also important to ask about the risk of nipple sensation loss or nipple necrosis, especially if skin excision is planned.
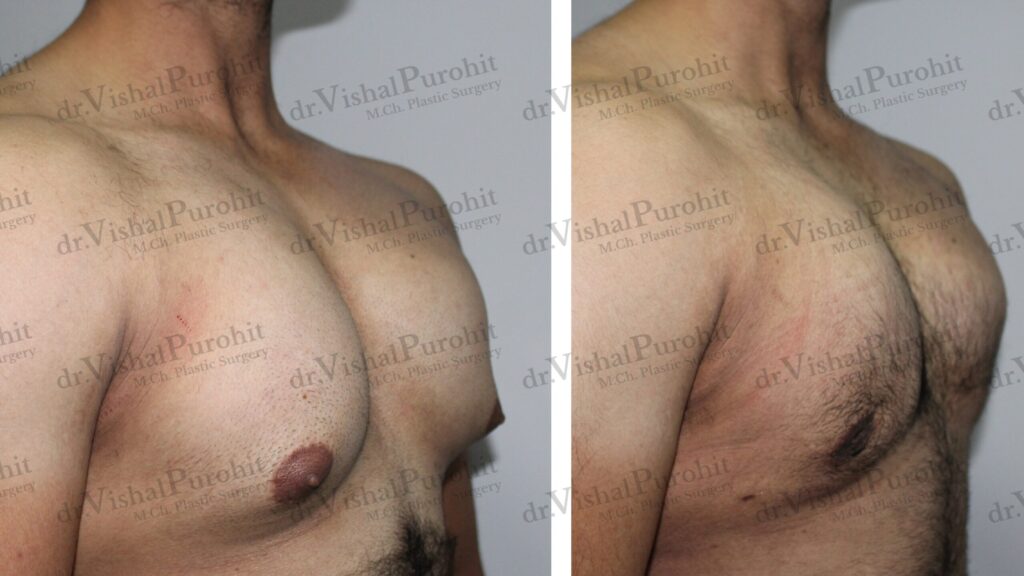
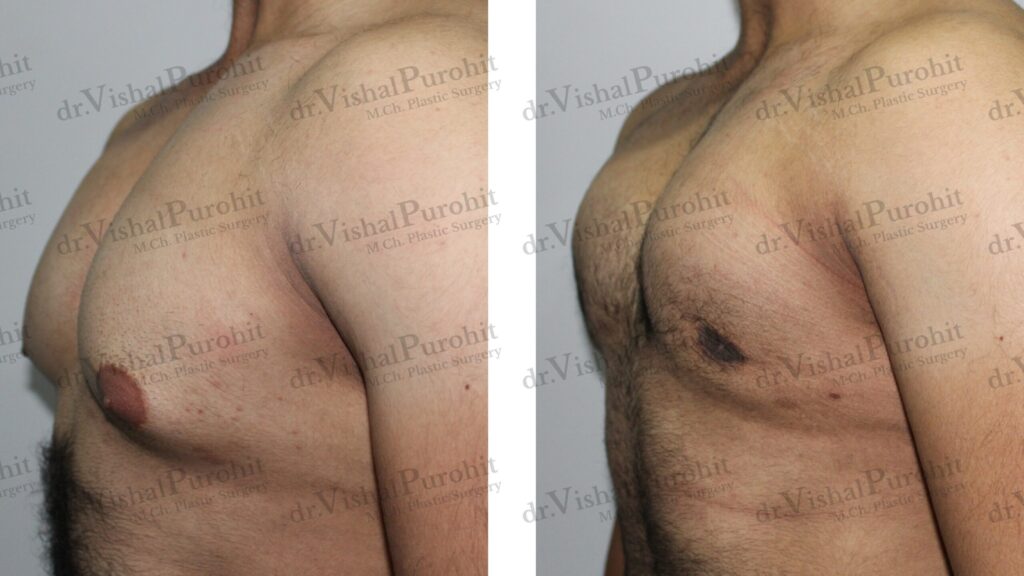
Questions regarding the aesthetic outcomes and scarring are essential. Ask where the incisions will be placed and what the resulting scars will look like, as the goal is often to achieve good aesthetic results with minimal scarring. You might also ask to see before-and-after photos of previous patients with similar grades of gynecomastia to gauge the surgeon’s expertise and aesthetic style.
Finally, ask about the recovery process and the long-term stability of the results. Inquire about the estimated recovery time, when you can return to normal activities or exercise, and the necessity of wearing compression garments. It is also wise to ask about the chance of recurrence; while rare with complete gland removal, understanding the risk factors for regrowth is important.
Take the First Step Today
Preparation is the key to a transformative result. If you are ready to start this journey with a board-certified expert who prioritises your safety, contact us today.
Dr. Vishal Purohit is ready to guide you from consultation to full recovery.
- 📞 Call/WhatsApp: +91 7718183535
- 📍 Visit Us: Kalpana Aesthetics, 2nd Floor, Jaipur Hospital, Mahaveer Nagar, Tonk Road, Jaipur
- 📅 Book Your Eligibility Consultation
Disclaimer: The content provided in this blog post is for informational and educational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider or board-certified plastic surgeon regarding your specific medical condition. Dr. Vishal Purohit is not liable for any decisions made based on this information.