When you are considering Gynecomastia Surgery in Jaipur, one of the first and most important steps in our consultation is diagnosis. Gynecomastia is not a uniform condition; its size, composition, and presentation differ dramatically between patients.
To create a precise, customised surgical plan, I use a standard grading system. Understanding which grade you fall into is the most important step in confirming your treatment plan, the cost of your surgery, and the benefits you can expect.
The Classification Challenge: Beyond Simple Size
While grading systems are essential, achieving an ideal classification system that guides surgeons precisely remains a challenge because objective assessment methods are generally absent from classification studies. This is largely because no single system is universally accepted.
The ideal classification system should be universal, surgically useful, and include a comprehensive set of clinically appropriate patient-related features, such as breast size, breast ptosis, tissue predominance, and skin redundancy. None of the current systems appears to fulfil all these criteria, necessitating a combined approach.
The Goal: There are many classification systems available, including Simon, Rohrich, and Wiesman. Some complex forms of gynecomastia do not match properly the existing classifications.
Modern Nuance: New systems, like the ultrasound-confirmed classification system, categorise types based on the most represented component (fat tissue, glandular tissue, or both) and the presence of ptosis, providing a more practical guide for surgeons.
The Simon Grades: A Foundational Roadmap
The most frequently referenced system is the Simon classification, which is based on surgical management after evaluating volume and skin surplus. It categorises patients into grades based on enlargement and skin excess:
| Simon Grade | Severity Description | Skin Characteristics |
| Grade I | Small enlargement – Puffy Nipple | No skin excess |
| Grade IIa | Moderate enlargement | No skin excess |
| Grade IIb | Moderate enlargement | Minor skin redundancy |
| Grade III | Marked enlargement | Marked skin redundancy |
Surgical Treatment Dictated by Grade
The severity grade dictates the required invasiveness and the necessary combination of techniques. A customised approach ensures that the surgical technique selected (liposuction, excision, or both) is the most effective and least invasive method for achieving a permanent, masculine chest contour.
Low Grades (I and IIa): Excision is Mandatory
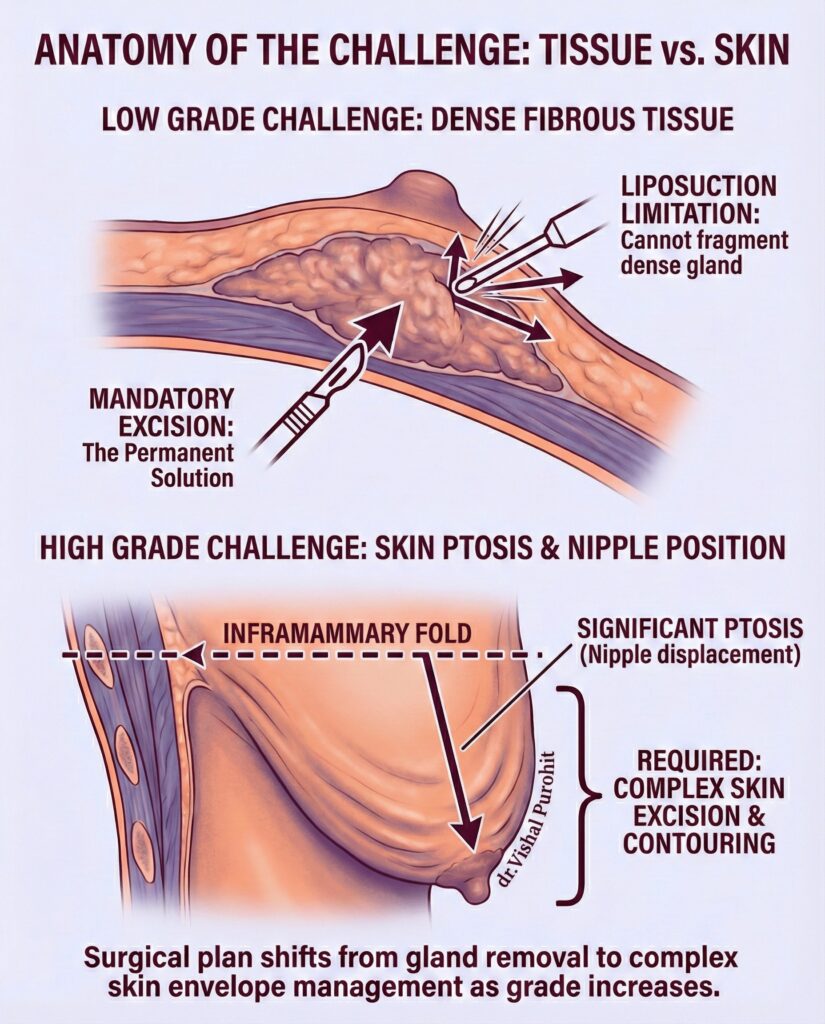
These grades involve minor to moderate enlargement with minimal or no skin excess. Although liposuction may be used to contour the surrounding area, glandular excision is critical for preventing recurrence.
Liposuction Limitations: Liposuction alone usually will not fully correct a significant proportion of gynecomastia cases. This happens because the dense fibrous glandular tissue is resistant to suction. For glandular hypertrophy, Liposuction alone usually will not fully correct a significant proportion of gynecomastia cases.
The Permanent Solution: Even for Grade I, if true glandular tissue is present, surgical excision of glandular tissue is considered essential to cure gynecomastia.
Technique for Grades I/II: For patients without significant skin excess, the pull-through technique is a safe and effective surgical option. Studies show this procedure can be done effectively via a single incision without the use of drains.
High Grades (IIb, III, and IV): Managing Skin Redundancy
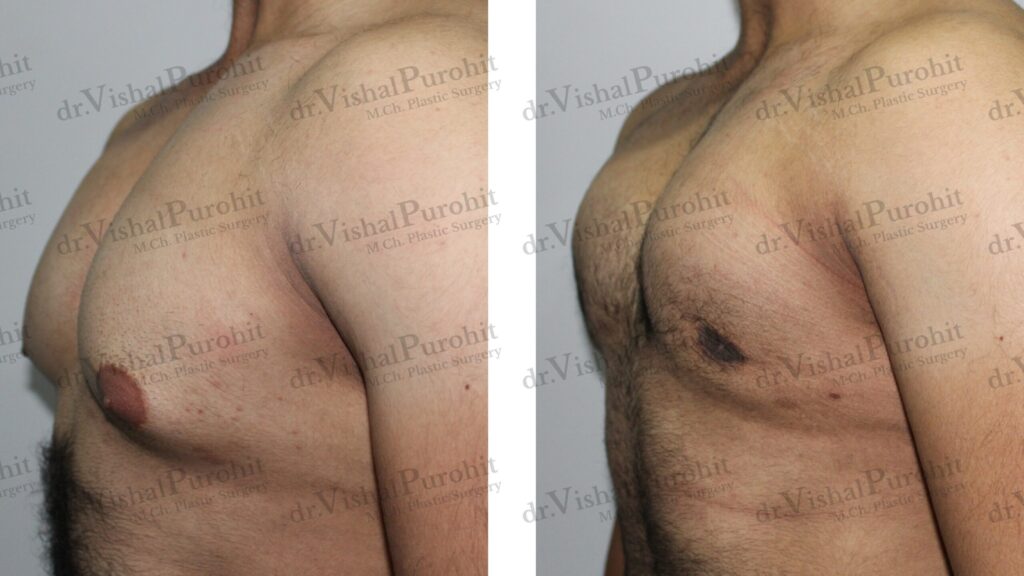
As the grade increases, the presence of significant skin redundancy (ptosis) and potential nipple displacement becomes the major technical challenge.
Defining Ptosis: Severity is often defined by the nipple-areola complex (NAC) position relative to the inframammary fold (IMF). Grade IV gynecomastia involves the NAC being more than 1 cm below the IMF.
Technique for Grade III
High-grade gynecomastia (Grade III) requires extensive tissue removal and often complex skin management. Techniques like the postero-inferior pedicle flap technique have been reported as promising for Grade III due to favourable functional and aesthetic results.
The Scar Trade-Off
For these advanced cases, the surgical plan must prioritise chest flatness and symmetry, which may increase scar visibility. The higher the grade of gynecomastia, the more complicated it is to form the male chest wall without leaving large, visible scars. The primary goal of surgery is the complete removal of the gland and excess skin, but for severe Grade III patients, the main surgical treatment is the free transplantation of the nipple–areola complex if the skin envelope cannot be adequately contracted.
Frequentlt Asked Questions
What are the different grades of gynecomastia, and how is each grade defined?
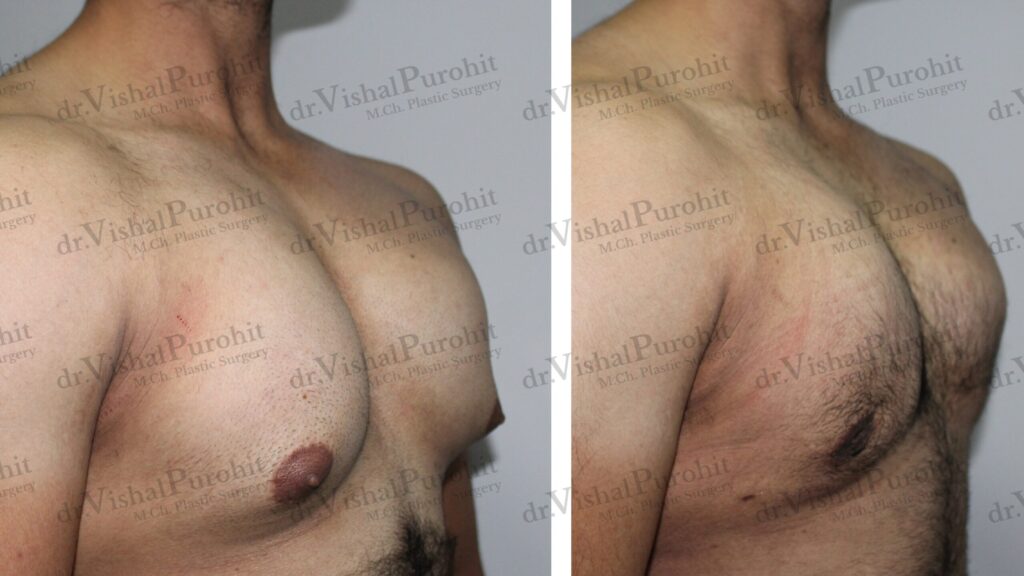
The most widely utilised system for categorising this condition is the Simon classification, which groups patients into four distinct categories based on the volume of breast tissue and the presence of excess skin. According to this system, Grade I is defined as a small, visible breast enlargement with no skin redundancy, while Grade IIa represents moderate breast enlargement, also without skin redundancy. These earlier grades are typically characterised by a localised button of tissue concentrated around the areola, making them easier to address surgically without extensive incisions.
As the severity of the condition progresses, the classification accounts for the elasticity and surface area of the skin envelope. Grade IIb is characterised by moderate breast enlargement accompanied by minor skin redundancy, indicating that the skin may not fully retract after tissue removal alone. This grade often serves as a borderline category where surgical decision-making becomes more complex regarding skin management.
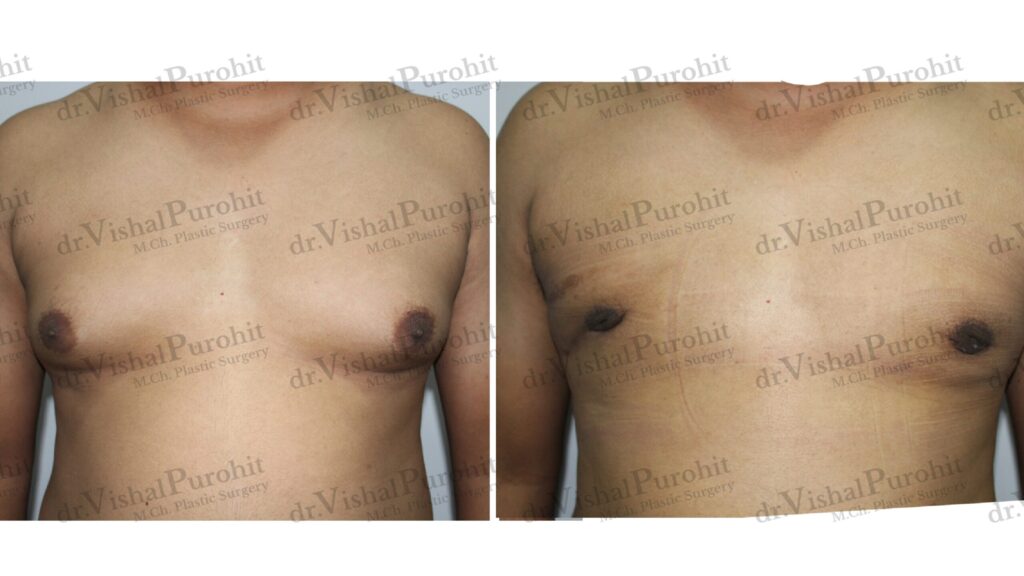
The most severe form, Grade III, involves gross or marked breast enlargement with significant skin redundancy that simulates a pendulous female breast. In these cases, the excess skin is a dominant feature, often requiring significant resection to achieve a flat chest contour. Some classification systems, such as the Rohrich classification, further stratify severe cases into Grade IV, which is defined by severe hypertrophy (often greater than 500 grams of tissue) combined with grade II or III ptosis (drooping) of the breast.
Other classification systems focus on the anatomical relationship between the nipple and the inframammary fold. For instance, the Cordova classification identifies Grade I as an increase in diameter limited to the areolar region, whereas Grade IV is defined by hypertrophy of all structural components where the nipple-areola complex is more than 1 cm below the inframammary fold. These varied definitions help surgeons precisely map the deformity to the appropriate surgical technique.
Which grades can typically be treated with liposuction alone, and which require gland excision or skin removal?
Treatment modalities are heavily dependent on the composition of the breast tissue (fatty vs. glandular) and the grade of the condition. Generally, Grade I and Grade IIa gynecomastia, which are characterised by minimal to moderate hypertrophy without skin redundancy, can often be treated effectively with liposuction alone or ultrasound-assisted liposuction (UAL), provided the tissue is predominantly fatty. However, if there is a significant fibrous glandular component, liposuction alone may be insufficient, and a direct pull-through surgical excision or open excision is required to remove the dense breast bud.
For Grade II b gynecomastia, where minor skin redundancy is present, the treatment plan becomes more nuanced. While some skin contraction can occur following ultrasound-assisted liposuction, patients with this grade often require surgical excision of the glandular tissue combined with techniques to manage the excess skin, such as a double donut mastectomy or circumareolar skin resection. In cases where the skin elasticity is poor, simple volume reduction may leave loose skin, necessitating a staged approach or immediate skin tightening.
Grade III and Grade IV gynecomastia almost invariably require more invasive surgical intervention involving both tissue removal and skin resection. These grades are characterised by marked enlargement and ptosis, meaning that skin-sparing techniques are no longer sufficient to flatten the thorax. Surgical management for these high-grade cases often resembles breast reduction patterns used in women, such as the inverted-T or vertical bipedicle techniques, to excise the redundant skin and reposition the nipple-areola complex.
In specific cases of pseudogynecomastia, which is defined as breast enlargement primarily due to adipose tissue without glandular proliferation, liposuction alone is often the definitive treatment regardless of size, as long as skin elasticity is adequate. However, surgeons must carefully palpate the breast post-liposuction to ensure no residual fibrous tissue remains, which would otherwise require excision to prevent a “puffy nipple” appearance.
How does the grade of gynecomastia affect expected scarring, surgical approach, and recovery time?
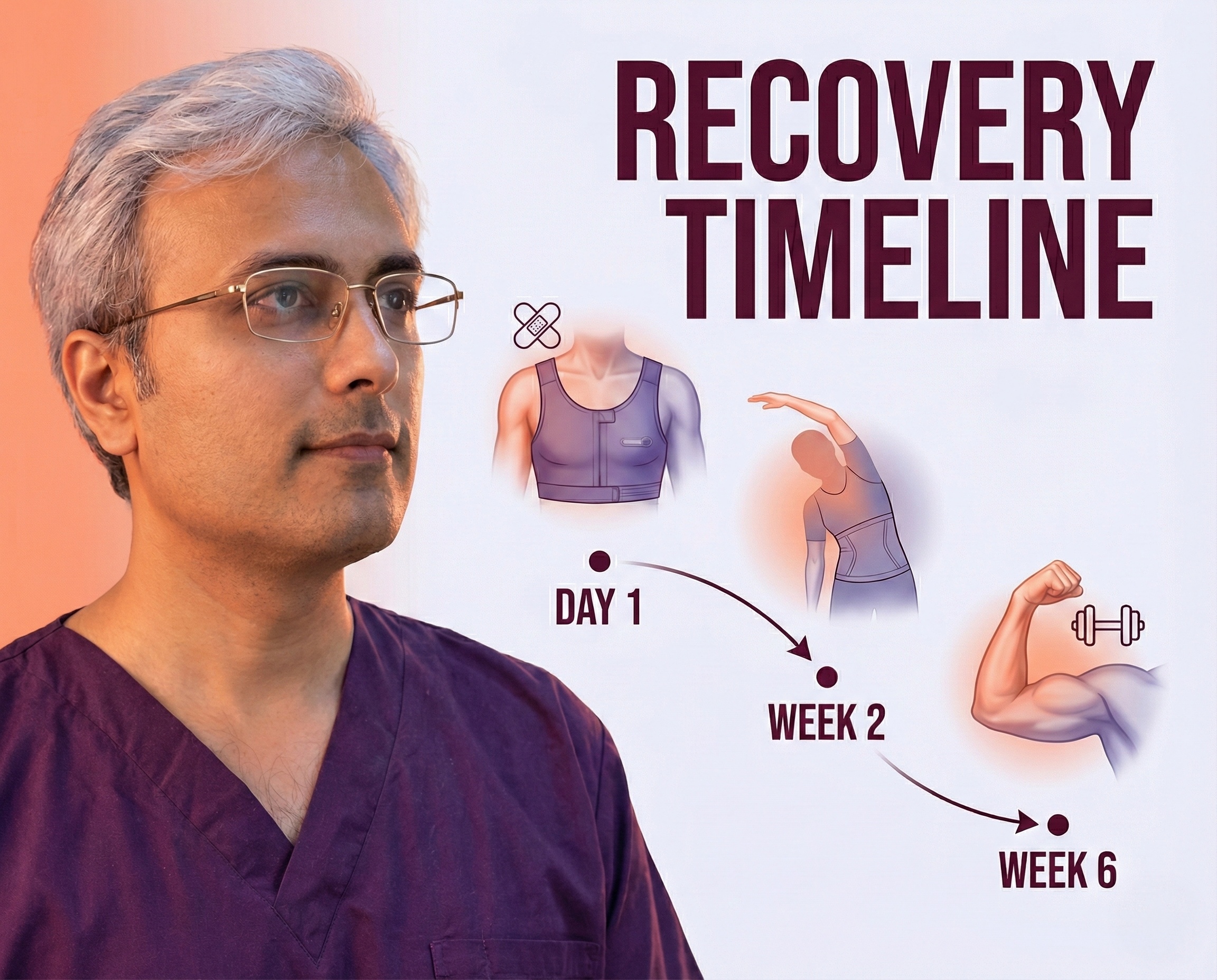
The grade of gynecomastia directly correlates with the invasiveness of the surgical approach and the resulting scarring. For Grade I and IIa cases, surgeries are typically minimally invasive, often utilising small stab incisions for liposuction or a small periareolar incision for pull-through excision. These techniques result in minimal, inconspicuous scars that are often well-hidden within the natural pigment lines of the areola or axilla.
As the severity increases to Grade IIb and III, the surgical approach must address skin redundancy, leading to more extensive scarring. Procedures to correct these grades often involve circumareolar incisions (around the entire areola) or even vertical and horizontal incisions (inverted-T) to remove excess skin and lift the nipple. Consequently, high-grade gynecomastia is associated with bigger scars and a higher likelihood of visible marks on the chest wall. Patients with Grade IV gynecomastia may even require free nipple grafts, which leave significant scarring and alter nipple sensation/pigmentation.
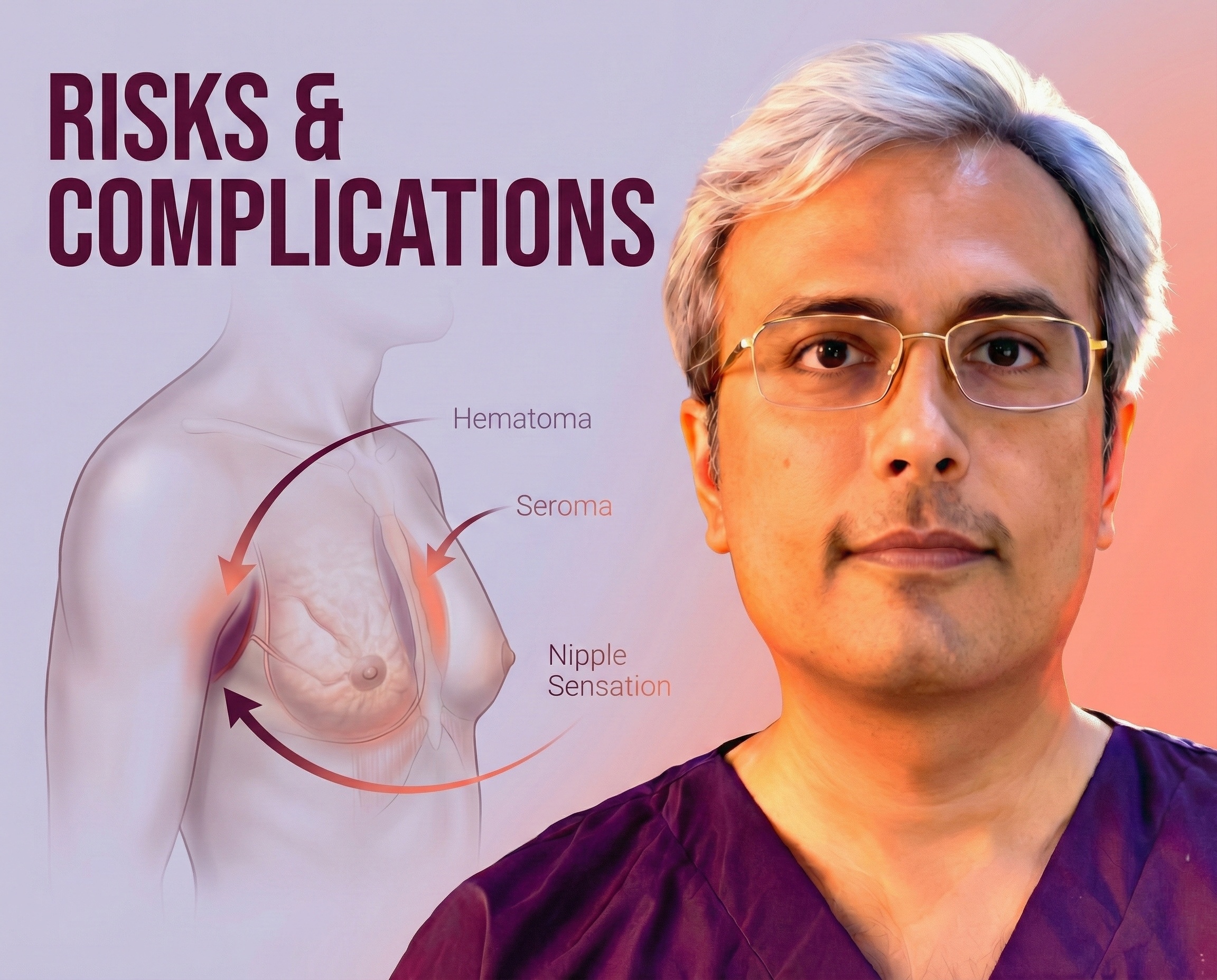
Recovery time and the risk of complications also scale with the grade of gynecomastia. Patients with higher grades (IIb, III, IV) undergoing extensive resection or skin removal have a higher risk of complications such as hematoma, seroma, and wound dehiscence. For example, one study noted that complications were exclusively observed in preoperative stages IIa–III, with higher rates in overweight patients. The recovery for these patients often involves longer periods of compression garment usage and restricted physical activity compared to those treated with liposuction alone.
Furthermore, the complexity of the surgical approach for high-grade gynecomastia can impact the aesthetic outcome, specifically regarding the nipple-areola complex (NAC). In severe cases involving ptosis, techniques like the superior pedicle NAC flap are used to reposition the nipple, which is a more intricate procedure than simple excision. This increases the operative time and the biological demand on the healing tissues, necessitating a more cautious postoperative recovery phase to ensure nipple viability.
Can early-grade gynecomastia (Grade I or II) be improved with lifestyle changes or medical treatment without surgery?
Early-grade gynecomastia, particularly when it is physiologic (pubertal) or of recent onset, has a high potential for improvement without surgery. Pubertal gynecomastia is often a self-limiting condition that resolves spontaneously in up to 90% of adolescents within 6 months to 3 years. Therefore, for Grade I or II cases in adolescents, a period of observation and reassurance is the primary recommendation before considering invasive interventions.
Medical treatment can be effective, but its success is time-dependent. Therapies using anti-estrogens like Tamoxifen or Danazol are most effective during the early proliferative phase, which typically lasts for the first 12 months. During this active phase, the glandular tissue is vascular and responsive to hormonal manipulation. Studies have shown that Tamoxifen leads to a significant reduction in breast size and pain in a majority of patients if treated early.
However, once the condition persists beyond one to two years, the tissue undergoes fibrosis and hyalinization, entering a quiescent, fibrous phase. At this stage, medical therapy may no longer be effective, and the glandular enlargement becomes irreversible. For patients with long-standing Grade I or II gynecomastia that has become fibrotic, surgery remains the only definitive treatment option, as the tissue will not respond to lifestyle changes or medication.
Lifestyle changes, specifically weight loss and exercise, are primarily effective for pseudogynecomastia (lipomastia), where the breast enlargement is due to adipose tissue rather than glandular proliferation. For patients with true glandular gynecomastia, weight loss may reduce the fatty component of the breast but will not eliminate the glandular tissue itself. In fact, significant weight loss can sometimes make the glandular tissue more apparent or lead to sagging pseudogynecomastia due to excess skin, potentially worsening the cosmetic appearance.
How does the grade of gynecomastia influence the cost and complexity of surgery?
The cost and complexity of surgery are directly proportional to the grade of gynecomastia. Low-grade gynecomastia (Grade I and IIa) is typically less complex to treat, often requiring only liposuction or a simple excision through a small incision. These procedures have shorter operative times, can sometimes be performed under local anaesthesia, and generally incur lower facility and surgical fees. The straightforward nature of these surgeries also translates to a lower risk of complications and revision, keeping the overall cost lower.
High-grade gynecomastia (Grade III and IV) significantly increases surgical complexity because it involves not just tissue removal but also skin reduction and nipple repositioning. Techniques such as the staged excision or mastopexy required for these grades take considerably longer to perform and demand a higher level of surgical expertise. The need for general anaesthesia, longer operating room time, and potentially an overnight hospital stay substantially increases the total financial investment for the patient.
Additionally, the likelihood of secondary procedures or revisions is higher in advanced grades. For instance, in cases of severe hypertrophy (Grade III/IV), patients may require a two-stage approach where ultrasound-assisted liposuction is performed first to allow for skin retraction, followed by a second surgery 6 to 9 months later to excise residual glandular tissue and skin. This multi-stage process naturally doubles the logistical complexity and financial cost compared to a single-stage intervention.
Finally, the complication profile associated with higher grades affects the overall “cost” in terms of recovery and potential additional treatments. High-grade corrections have a statistically significant increase in complications such as hematoma or wound dehiscence, particularly in resections exceeding 40 grams or in overweight patients. Managing these complications may require further medical attention, expanding the total cost and recovery burden for the patient.
Your Consultation in Jaipur
Your specific gynecomastia grade dictates the complexity and cost of your surgery. To get an accurate diagnosis and determine which grade defines your chest enlargement, I invite you to consult with me.
To book your personalised, confidential consultation, please reach out to my team at Kalpana Aesthetics.
- Call or WhatsApp: 7718183535
- Visit Us: Kalpana Aesthetics, 2nd Floor, Jaipur Hospital, Mahaveer Nagar, Tonk Road, Jaipur
Disclaimer: The information provided on this webpage is for educational purposes only and does not constitute medical advice. The gynecomastia grading system is a tool used by medical professionals to classify severity. Only a qualified, board-certified plastic surgeon can provide an accurate diagnosis after a physical examination. Individual results and surgical needs will vary.