If you are struggling with the appearance of your chest, the first and most important step is to get a clear, medical diagnosis. Many men feel self-conscious about this condition, but it is crucial to know that “man boobs” are a recognised medical issue, not a personal failing.
While understanding the causes is vital, many patients ultimately find that the most effective solution is surgical intervention. Dr Vishal Purohit specialises in Gynecomastia Surgery in Jaipur, offering a permanent path to restoring a masculine chest contour. In this guide, we will break down exactly what this condition is, why it occurs, and how to distinguish it from simple weight gain.
Gynecomastia is one of the most common disorders affecting adolescent and adult males. It is defined as the benign proliferation of glandular breast tissue, characterised by a firm disc of tissue underlying the nipple.
In this comprehensive guide, we will break down exactly what this condition is, why it occurs, and how to distinguish it from simple weight gain.
Dr. Vishal Purohit’s Insight:
“I want to be very clear: gynecomastia is a medical condition. It is almost always caused by factors outside of your control, like hormones, medications, or genetics. Understanding the root cause is the first step toward finding the right, permanent solution.”
What Is Gynecomastia? (The Medical Definition)
Gynecomastia (often colloquially called “man boobs”) is the enlargement of male breast tissue.
What most people don’t know is that both men and women have breast glands. While in women, they are very well developed, in men, they are usually rudimentary (underdeveloped). However, under certain conditions, these glands can grow.
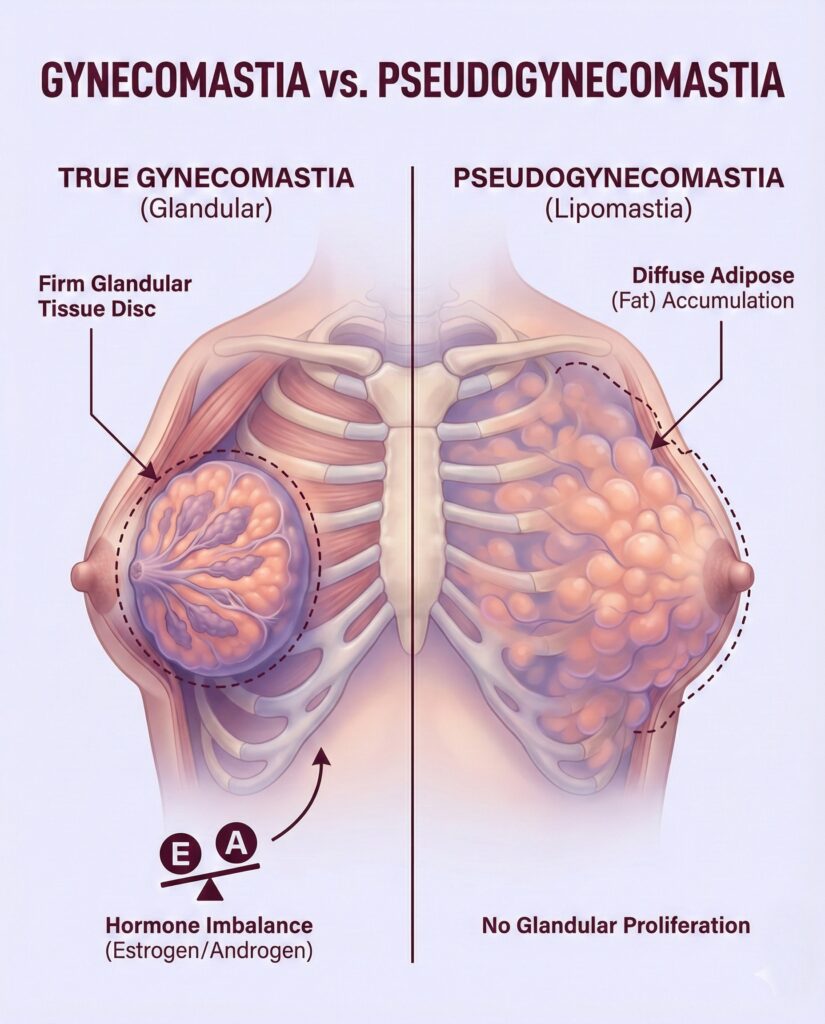
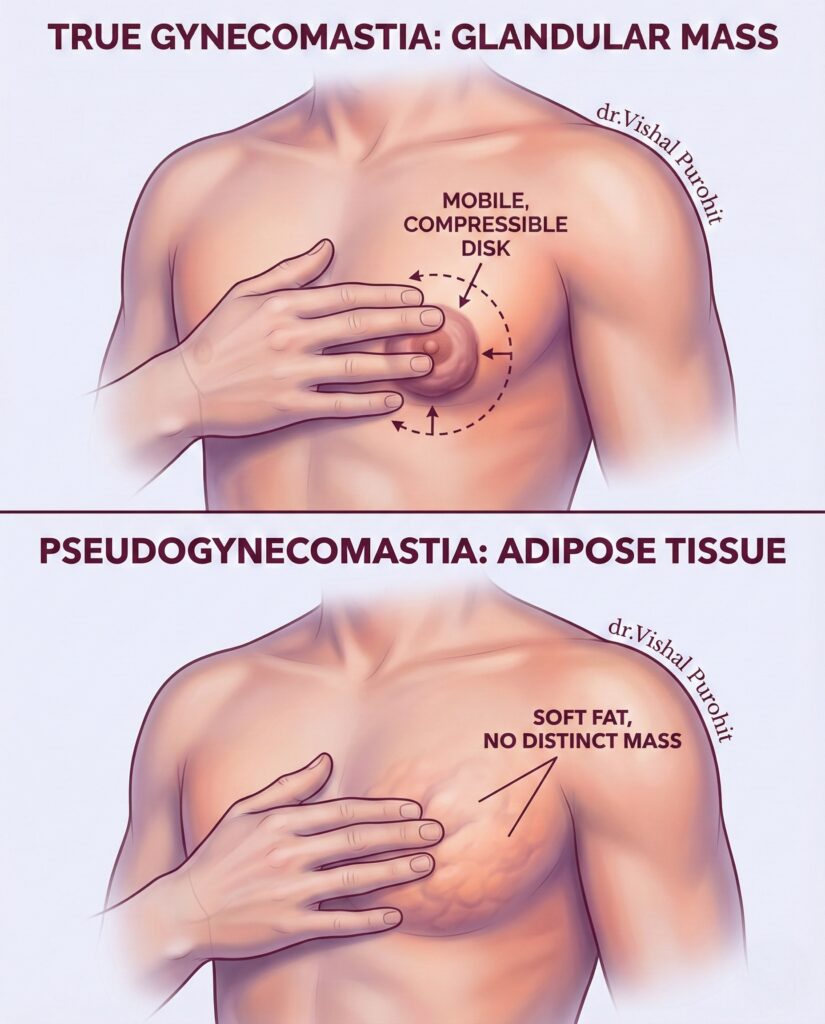
True Gynecomastia vs. Pseudo-Gynecomastia
It is vital to distinguish between two very similar-looking conditions:
- True Gynecomastia: This involves the growth of glandular tissue (firm, rubbery tissue under the nipple). It cannot be exercised away.
- Pseudo-Gynecomastia (Lipomastia): This is caused purely by excess fat deposition in the chest area due to obesity. This often responds to diet and exercise.
Do you need surgery?
If you have true glandular gynecomastia, medical or surgical intervention is usually required. If you are unsure about your eligibility, you can read our guide on Candidacy & Eligibility for Surgery.
Why Does It Occur? The Root Causes
When seeking treatment, understanding the root cause is the first step. Male breast enlargement is almost always traceable to fundamental shifts in the body’s chemical messengers.
The Core Mechanism: Hormonal Imbalance
The underlying mechanism of true gynecomastia is a hormonal disparity. The condition is caused by an altered ratio of estrogens (female hormones) to androgens (male hormones).
While men primarily produce testosterone, they also produce small amounts of estrogen. If this balance shifts—either due to a drop in testosterone or a spike in estrogen—breast tissue is stimulated to grow.
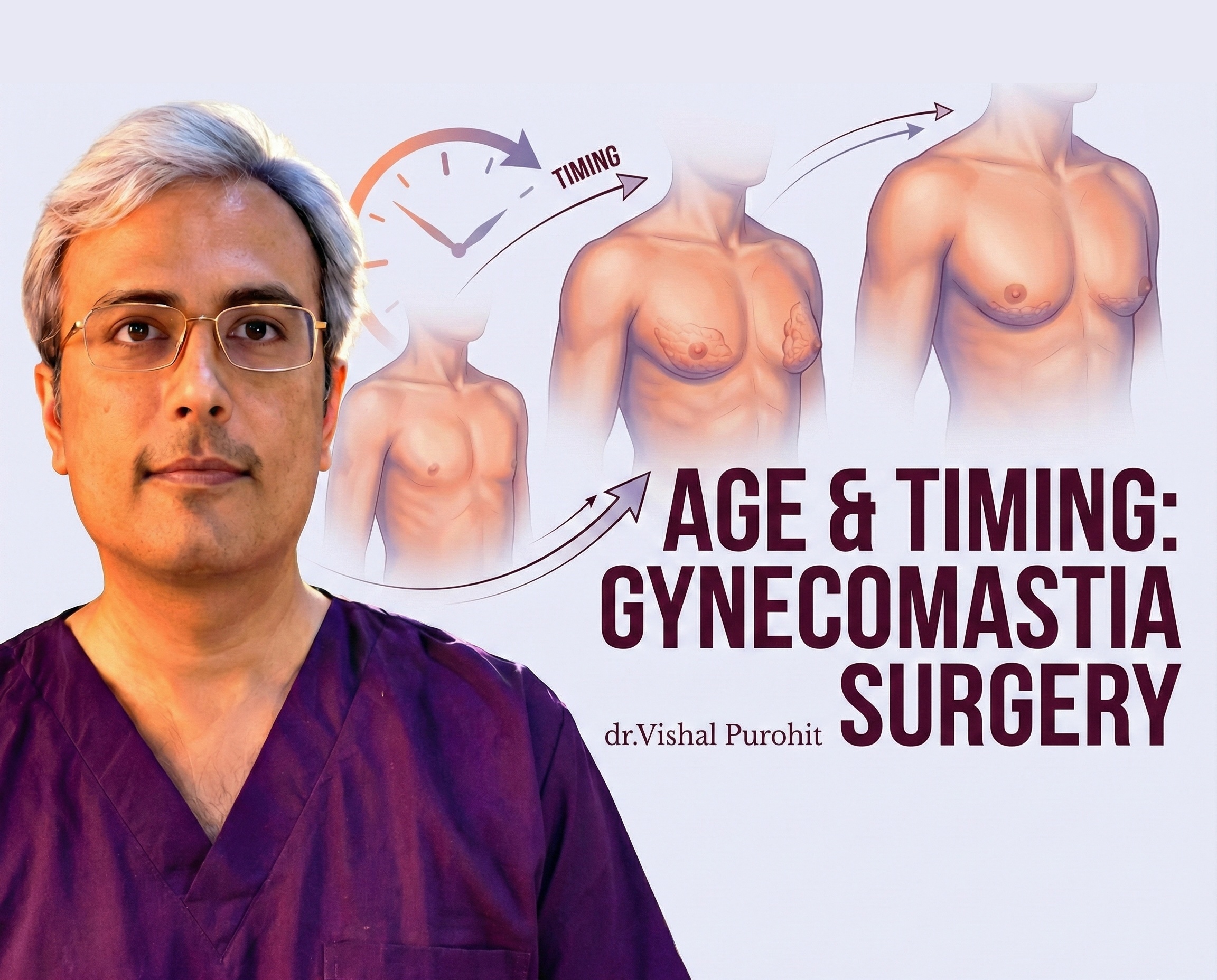
Common Triggers by Age Group
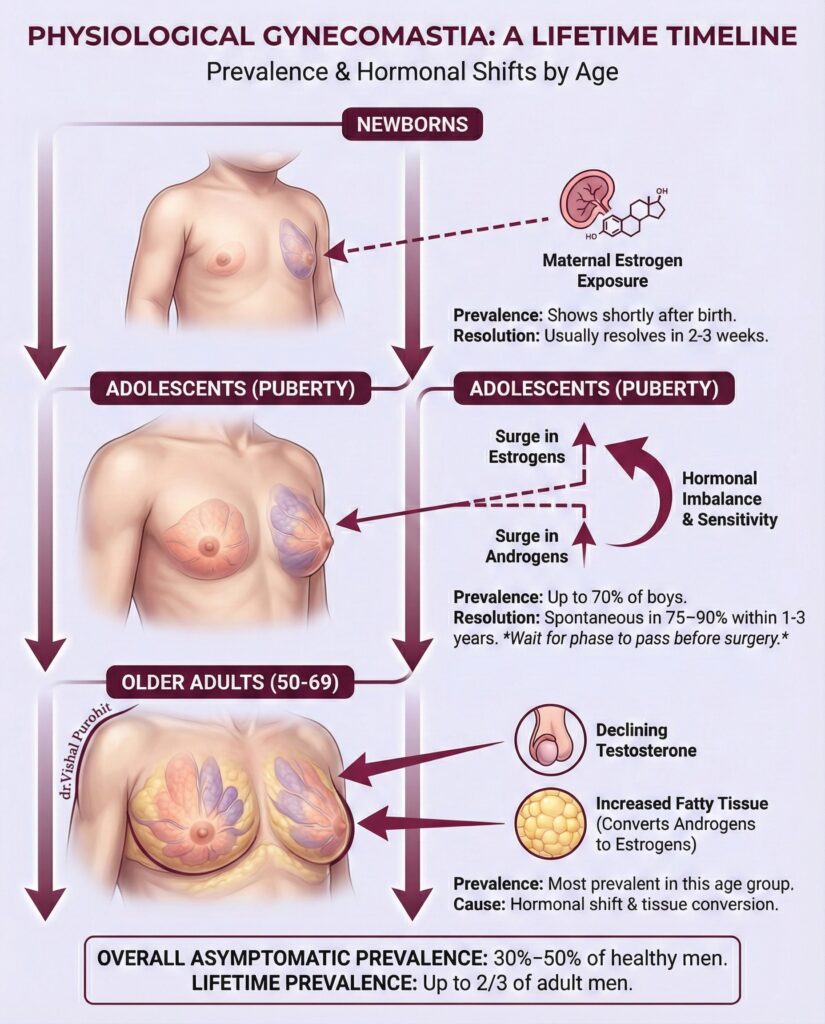
Puberty (Physiologic Gynecomastia)
During puberty, a boy undergoes many physiological changes. Sometimes, there is a transient imbalance in hormonal levels.
- The Stats: In up to 60% of boys, there is a noticeable increase in male breast tissue.
- The Outlook: In most cases, this is temporary. As hormone levels stabilise, the glands often flatten out. However, for a small percentage, the glands remain permanent into adulthood.
Learn more about how age affects treatment here: Adolescents: Age & Timing for Surgery.
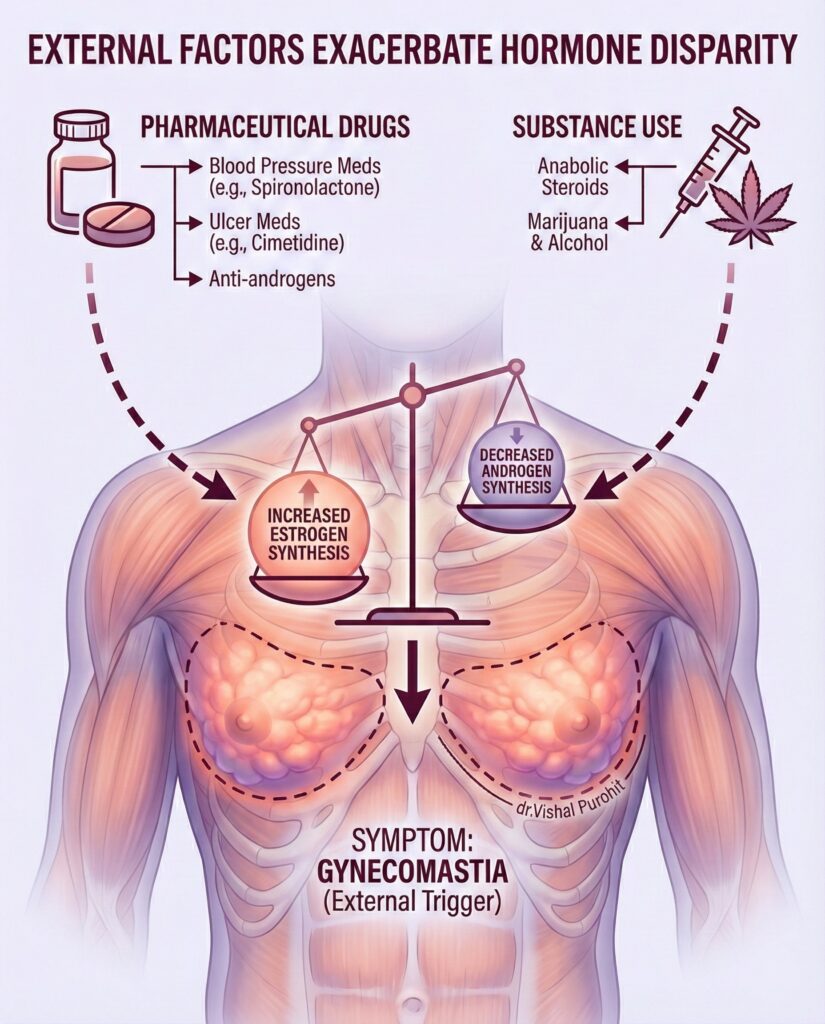
Medication-Induced Gynecomastia
Certain medications can disrupt your hormonal balance. Common culprits include:
- Anti-androgens (used for prostate conditions).
- Anabolic steroids (often used for bodybuilding).
- Certain anti-anxiety and heart medications.
Obesity & Lifestyle
Fat cells contain an enzyme called aromatase, which converts testosterone into estrogen. Therefore, significant weight gain can create a cycle where excess fat leads to higher estrogen, which promotes breast tissue growth.
Read more: Gynecomastia & Weight Loss: The Connection
Chronic Health Issues Create Hormonal Imbalance
Sometimes, gynecomastia may present as a symptom of an underlying chronic disease that is disrupting your hormone metabolism or production. This is why a full medical check-up is mandatory.
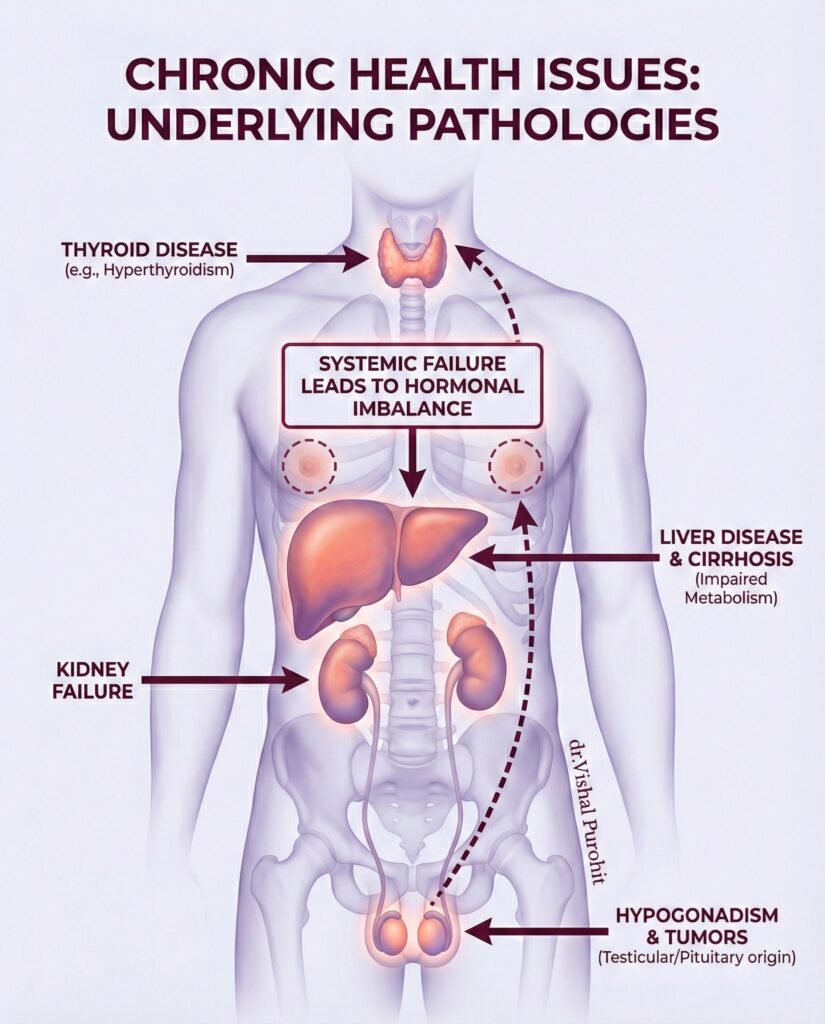
A key part of your consultation will be running diagnostic tests to rule out these underlying pathologies:
- Liver Disease and Cirrhosis: Liver failure impairs the body’s ability to properly metabolise hormones like estrogen.
- Kidney Failure: Many kidney failure patients experience a hormonal imbalance.
- Hypogonadism: This condition, caused by damage to the testes or pituitary, leads to a deficiency in androgen (testosterone) production.
- Thyroid Disease: Conditions like hyperthyroidism can cause hormonal imbalance.
- Tumours: Estrogen excess can be because of a variety of causes, including testicular estradiol production (Sertoli or Leydig cell tumours) or hCG-secreting tumours.
The Symptoms: What to Look For
How do you know if you have gynecomastia? Look for these signs:
- Swelling: A “puffy” appearance of the nipple or areola.
- Tenderness: The tissue directly under the nipple may feel tender or sore to the touch.
- Texture: You may feel a firm, rubbery lump (the gland) distinct from the surrounding soft fat.
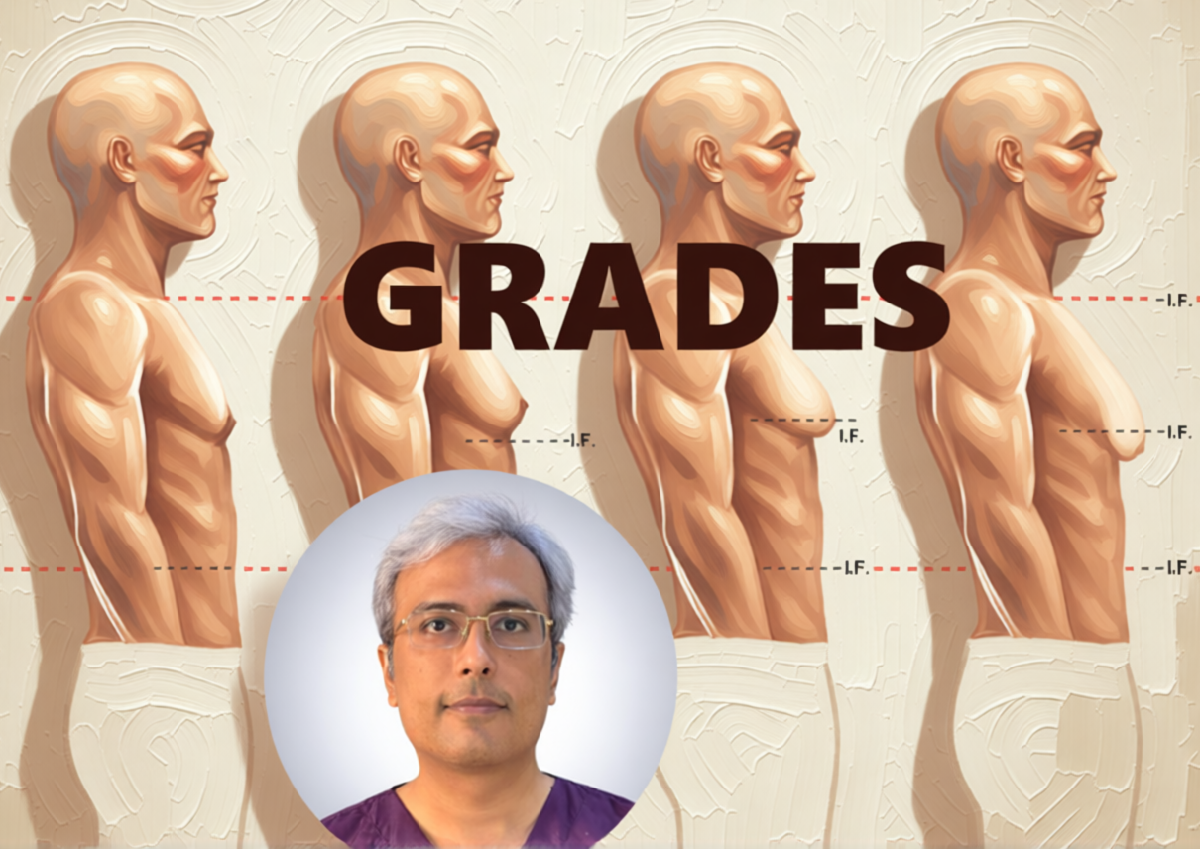
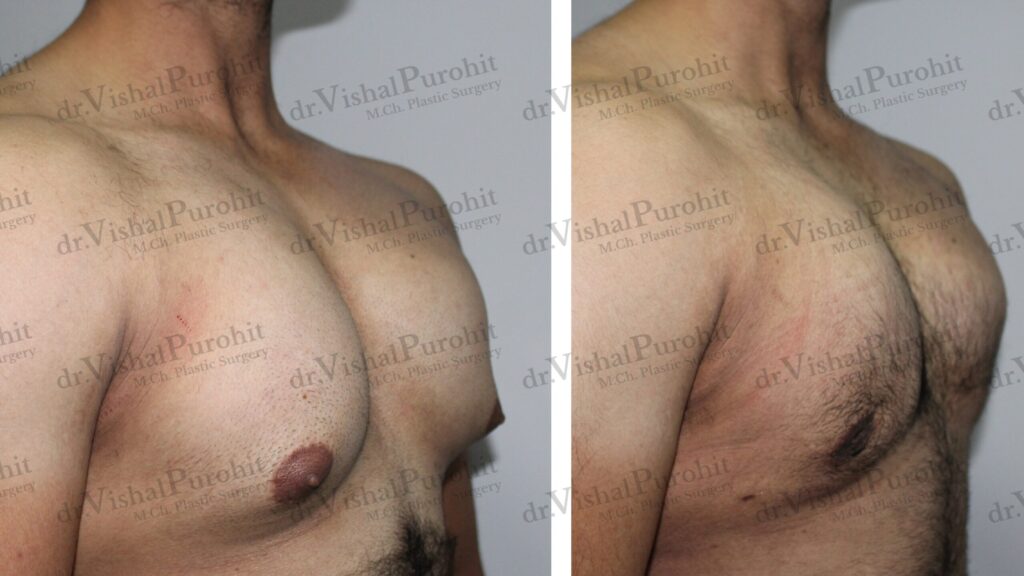
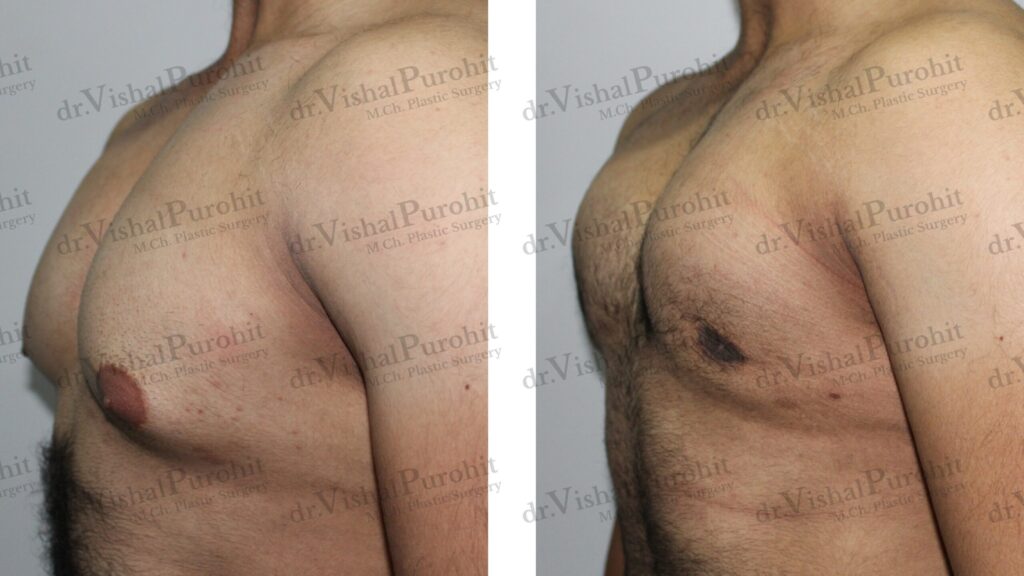
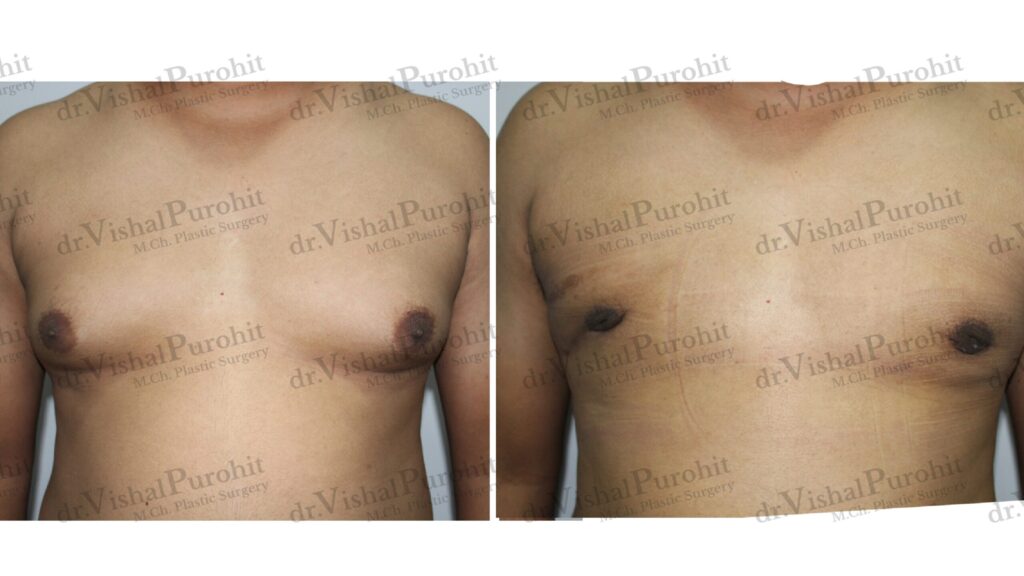
The 4 Grades of Gynecomastia
Surgeons classify the severity of the condition to determine the best surgical approach. This grading also heavily influences the cost of Gynecomastia Surgery.
- Grade 1: Minor enlargement, primarily a “puffy nipple” with no excess skin.
- Grade 2: Moderate enlargement extending beyond the areola, but with no excess skin.
- Grade 3: Moderate enlargement with some excess skin.
- Grade 4: Marked enlargement resembling a female breast, with significant excess skin.
This detailed post on Grades of Gynecomastia will clarify any further confusion.
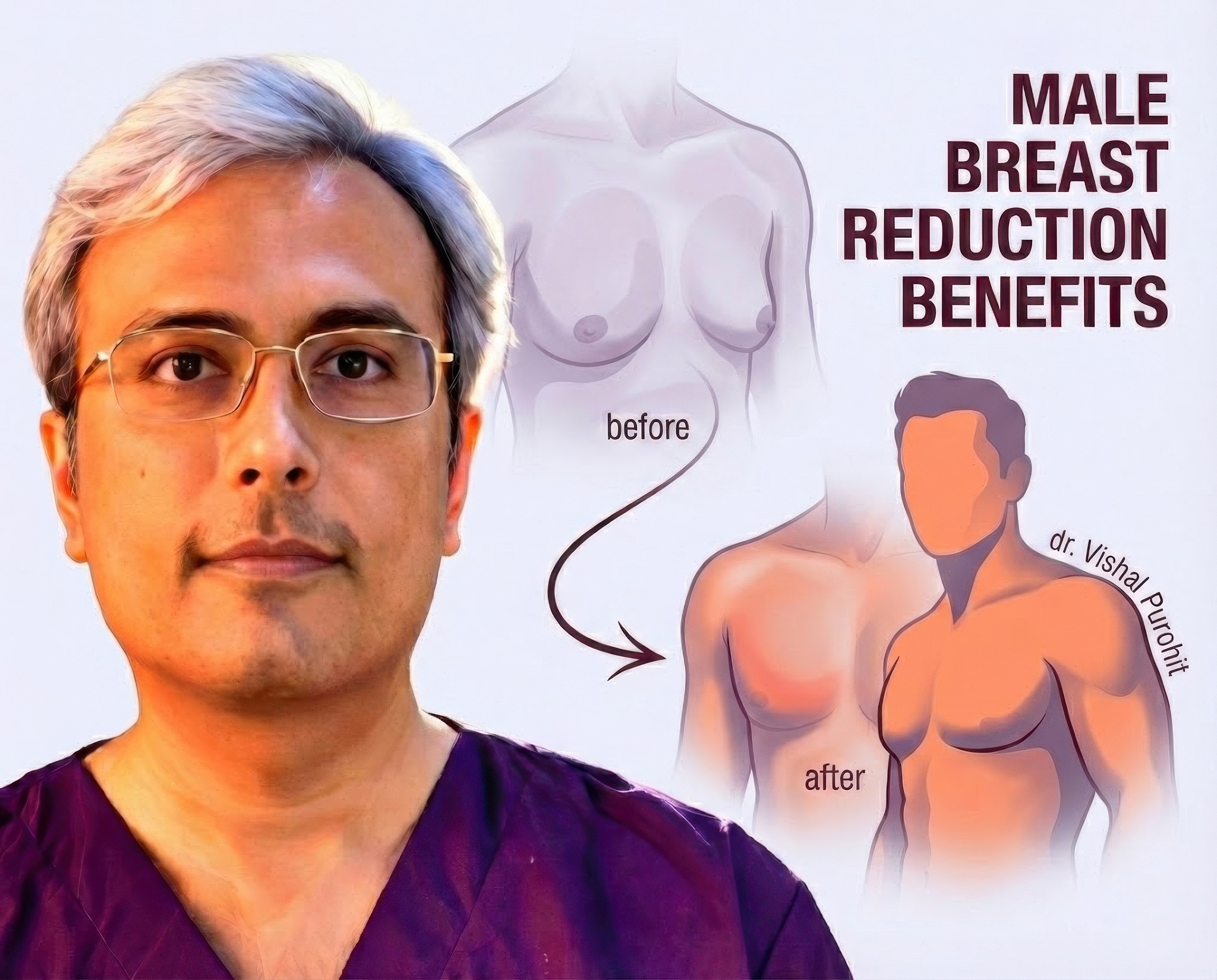
Is It Treatable?
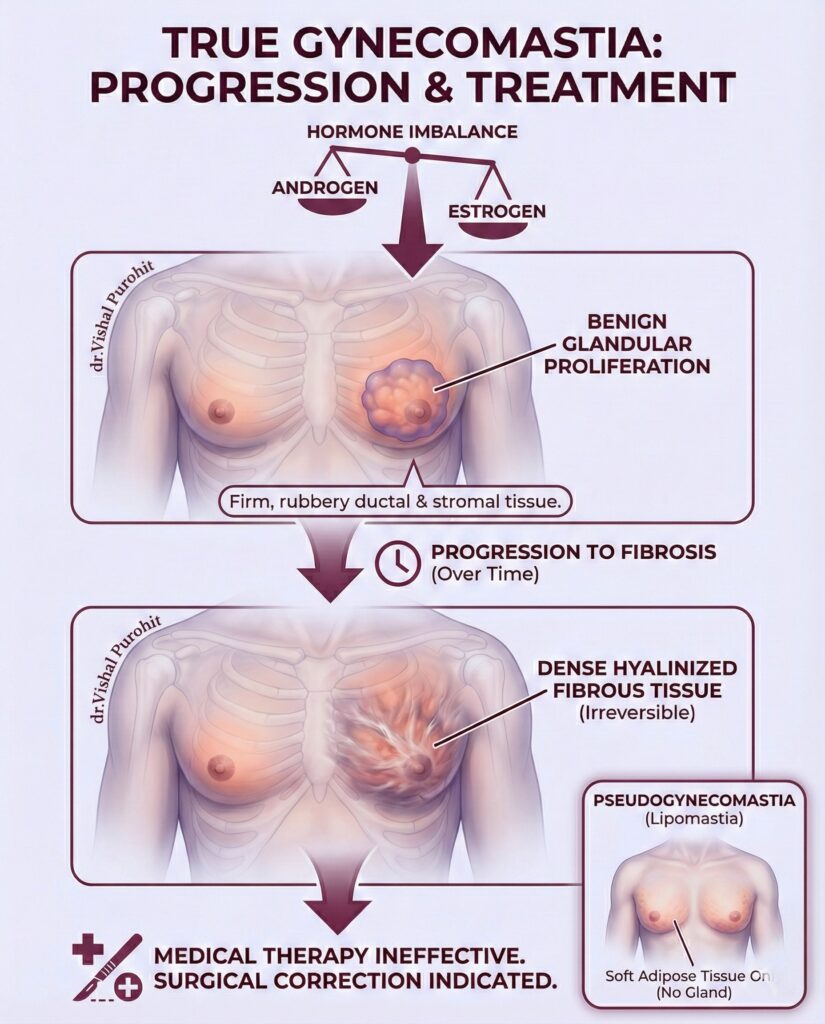
Yes. While pubertal gynecomastia may resolve on its own, established glandular tissue in adults rarely disappears without intervention.
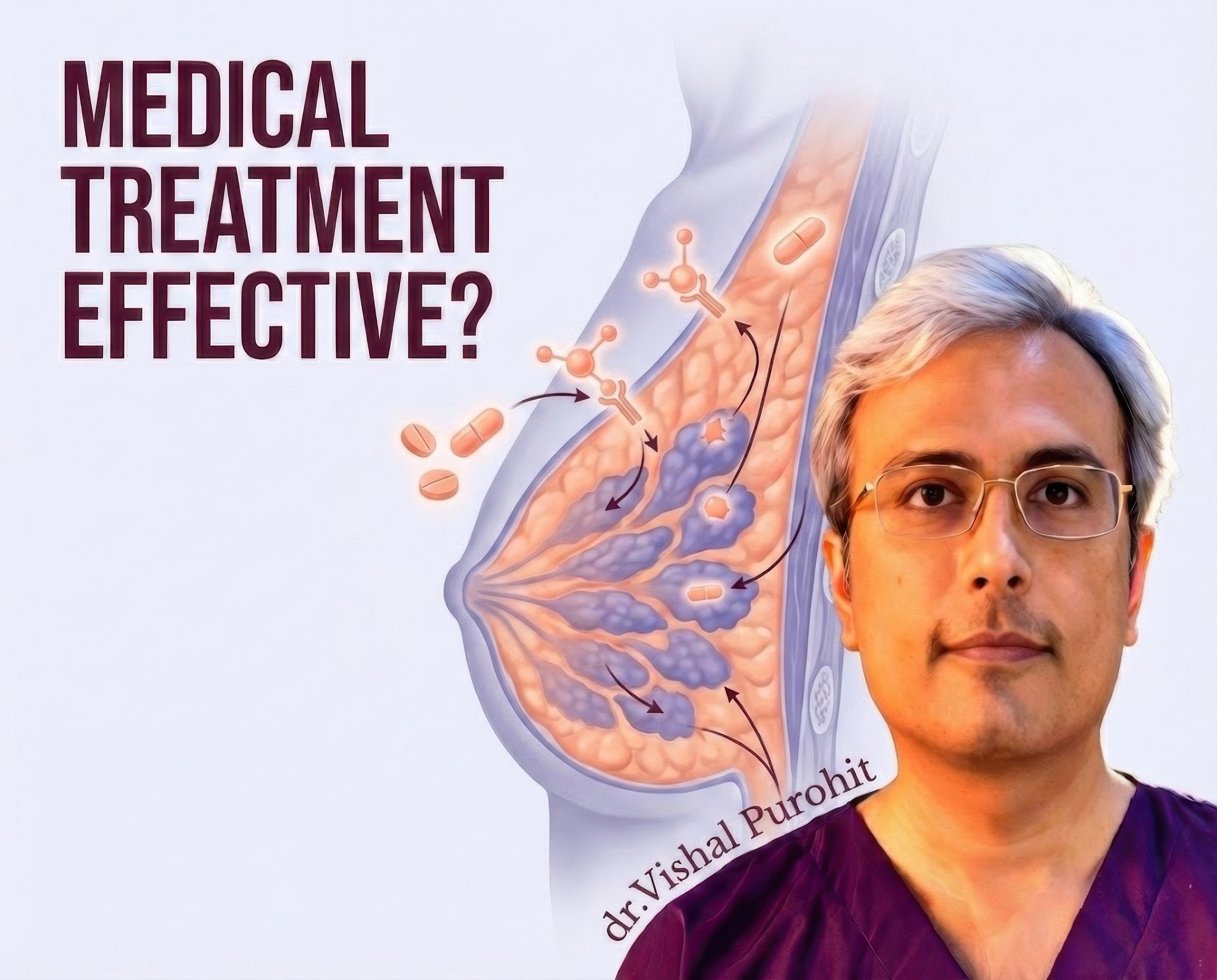
- Medical Treatment: In very early stages (the “painful” phase), certain medications may help reduce size. See: Medical Management vs. Surgery.
- Surgical Treatment: For established cases, the gold standard is Gland Excision with Liposuction. This physically removes the gland and contours the chest for a permanent result.
Ready to Restore Your Confidence?
If you suspect you have gynecomastia, you don’t have to live with it. A consultation can confirm the diagnosis and rule out other issues.
Frequently Asked Questions
What is gynecomastia, and how does it differ from pseudogynecomastia?
Gynecomastia is defined as the benign enlargement of the male breast tissue, resulting from the proliferation of the glandular component. It is the most common breast condition in men, often presenting as a rubbery or firm mass extending concentrically from the nipple. This condition is distinct because it involves the actual development of breast ducts and stroma, rather than just adipose tissue. It can occur unilaterally or bilaterally and is frequently associated with breast pain or tenderness, particularly in its early stages. The prevalence of this condition varies, affecting a significant portion of the male population at different life stages, including neonates, adolescents, and older men.
In contrast, pseudogynecomastia, also known as lipomastia, is characterised by the accumulation of subareolar fat without enlargement of the glandular tissue. This condition is clinically similar in appearance to true gynecomastia but is fundamentally different in its tissue composition. Pseudogynecomastia is most commonly observed in obese men, where increased total body fat leads to fat deposition in the chest area. Unlike true gynecomastia, the enlarged breast mound in pseudogynecomastia is soft to palpation and lacks the firm, discoid tissue characteristic of glandular growth.
Distinguishing between these two conditions is critical for appropriate management. Physical examination plays a key role; true gynecomastia presents as a palpable, firm ridge of tissue, whereas pseudogynecomastia feels consistent with the surrounding fatty tissue. When physical examination is inconclusive, imaging modalities such as breast ultrasonography can effectively differentiate between the dense glandular tissue of true gynecomastia and the radiolucent fat of pseudogynecomastia. Ultrasound can visualise the specific subareolar nodule or flame-shaped tissue indicative of glandular proliferation.
The distinction determines the surgical approach if treatment is required. Pseudogynecomastia is often treated effectively with liposuction alone, as the primary issue is adipose tissue. True gynecomastia, however, typically requires the surgical removal of the fibroglandular breast tissue, often in combination with liposuction to achieve a contoured result. Failure to identify the glandular component can lead to incomplete treatment and patient dissatisfaction if only liposuction is performed on a patient with true glandular hypertrophy.
What are the common causes and risk factors for developing gynecomastia?
The primary pathophysiological mechanism behind gynecomastia is an imbalance of androgens and estrogens, where the stimulatory effects of estrogen on breast tissue override the inhibitory effects of androgens. This hormonal disruption can be caused by a decrease in testosterone production, an increase in estrogen production, or an increase in the conversion of androgens to estrogens by the enzyme aromatase. Physiological gynecomastia is common and occurs during three distinct life phases: the neonatal period due to maternal estrogens, puberty due to transient hormonal fluctuations, and old age due to declining testosterone levels and increased adiposity.
Pathological causes are varied and can include systemic illnesses and endocrine disorders. Conditions such as liver cirrhosis, renal failure, and hyperthyroidism are known to alter hormone metabolism and binding proteins, leading to breast enlargement. Furthermore, testicular tumours (such as Leydig cell tumours) or adrenal tumours can directly secrete estrogens or precursors, while pituitary disorders may lead to secondary hypogonadism. Genetic conditions like Klinefelter syndrome are also significant risk factors, representing a form of primary hypogonadism associated with gynecomastia and an increased risk of male breast cancer.
Medications and recreational drugs are a frequent cause of non-physiological gynecomastia. A wide array of drugs has been implicated, including anti-androgens used for prostate cancer, spironolactone, cimetidine, and certain heart medications like digoxin. Recreational substances such as alcohol, marijuana, and heroin can also disrupt hormonal balance. Notably, the use of anabolic steroids by athletes and bodybuilders is a well-documented cause, as exogenous androgens can be aromatised into estrogens, stimulating breast tissue growth.
Risk factors such as obesity play a dual role. Adipose tissue contains the aromatase enzyme, which converts testosterone into estradiol, thereby increasing systemic estrogen levels. Consequently, increased body mass index (BMI) is strongly correlated with the prevalence of gynecomastia. Additionally, ageing is a significant risk factor; as men age, testosterone levels naturally decline while SHBG (sex hormone-binding globulin) levels rise, reducing the amount of free, biologically active testosterone available to inhibit breast tissue proliferation.
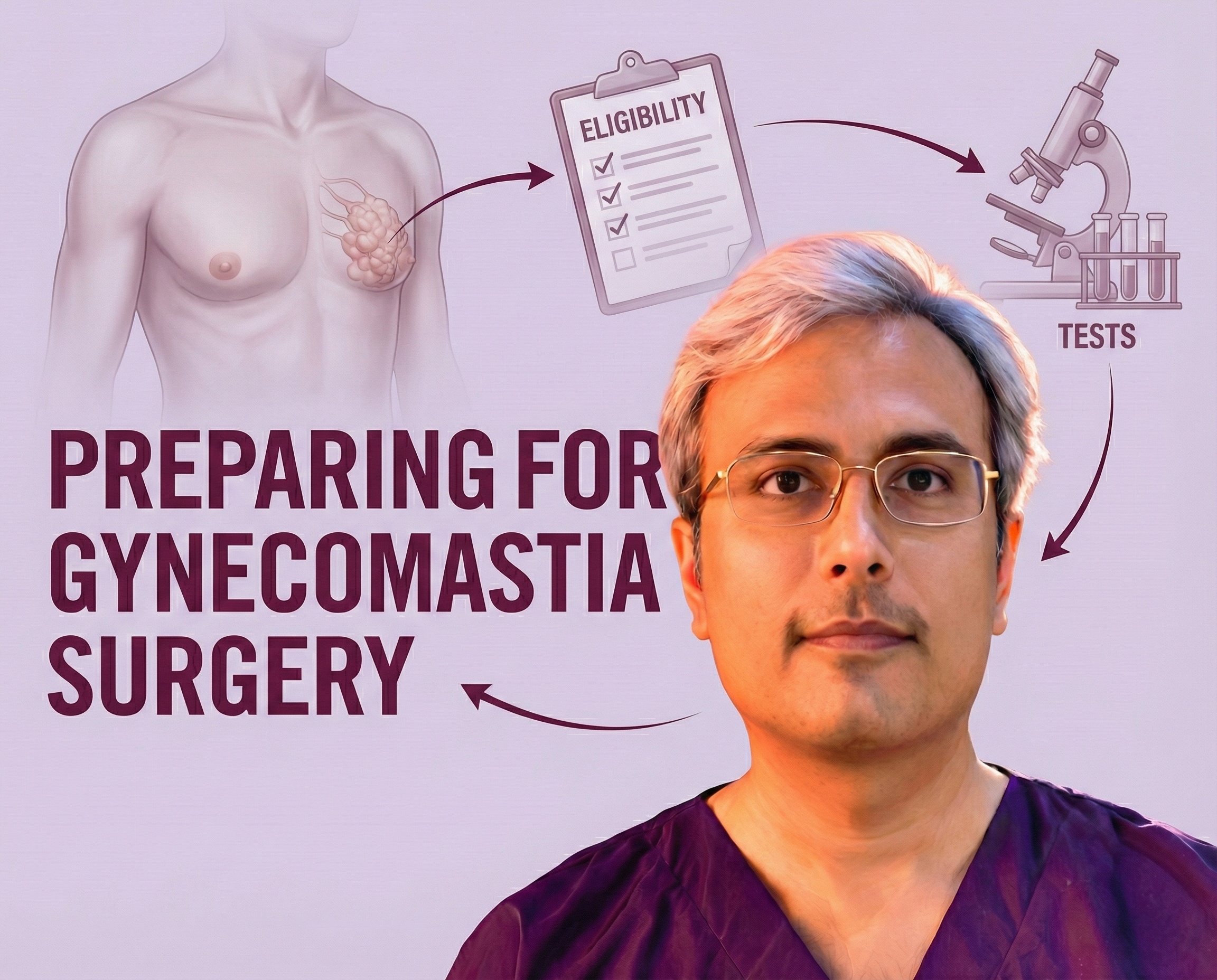
How is gynecomastia diagnosed, and which tests are needed before treatment?
The diagnostic evaluation of gynecomastia begins with a detailed history and physical examination. The history should focus on the duration of breast enlargement, the presence of pain or tenderness, and any changes in testicular size. It is crucial to review a complete list of medications and recreational drugs, as drug-induced gynecomastia is common. The physical exam involves palpating the breast to distinguish the firm, concentric glandular tissue of gynecomastia from the soft adipose tissue of pseudogynecomastia and checking for signs of malignancy, such as hard, eccentric masses or skin changes.
Laboratory investigations are tailored based on the clinical findings. For adolescents with typical pubertal gynecomastia or adults with long-standing, asymptomatic enlargement, extensive testing may not be necessary. However, if the condition is of recent onset, progressive, or symptomatic, a hormonal workup is indicated. This typically includes measuring serum levels of testosterone, estradiol, luteinizing hormone (LH), follicle-stimulating hormone (FSH), prolactin, and human chorionic gonadotropin (hCG) to rule out testicular or pituitary tumours. Liver and kidney function tests may also be included to exclude systemic metabolic causes.
Imaging studies serve as an adjunct to physical examination. Breast ultrasonography is the primary imaging modality used to confirm the presence of glandular tissue and differentiate it from fatty deposition. It is particularly useful when the physical exam is equivocal. Mammography may be utilised if there is a suspicion of breast cancer, particularly in older men or those with asymmetric, hard lumps. Testicular ultrasound is recommended if a testicular mass is suspected or if there are elevations in serum estradiol or hCG.
Pathologic examination of the excised tissue is generally performed after surgery to rule out occult malignancy, although this practice has been debated for routine cases in adolescents. While the incidence of malignancy in gynecomastia specimens is extremely low, especially in young patients, histological analysis can confirm the benign nature of the proliferation. In cases where the clinical picture is suspicious or in older patients, biopsy prior to surgery may be indicated, although it is not standard for typical gynecomastia.
What treatment options are available, and when is surgery recommended?
The management of gynecomastia depends on the aetiology, duration, and severity of the condition. For physiological cases, such as pubertal gynecomastia, observation and reassurance are often the first line of treatment, as the condition frequently resolves spontaneously within one to two years. If a reversible cause is identified, such as a specific medication, discontinuing the offending agent may lead to regression. Medical therapy with anti-estrogens like Tamoxifen or aromatase inhibitors has been used, particularly in the early, proliferative phase of the disease, but these are less effective once the tissue has become fibrotic.
Surgery is recommended when gynecomastia persists for more than 12 months, as the tissue typically undergoes irreversible fibrosis and hyalinization, making medical therapy ineffective. Surgical intervention is also indicated for patients who experience significant pain, tenderness, or psychosocial distress due to the appearance of their chest. The primary goal of surgery is to restore a normal male chest contour and alleviate the emotional burden associated with the deformity.
Surgical options include a variety of techniques ranging from minimally invasive procedures to open excision. Liposuction-assisted surgery is effective for removing the fatty component of the breast and can be sufficient for patients with pseudogynecomastia or mixed types where the glandular component is minimal. However, for true gynecomastia with dense fibrous tissue, liposuction alone is often inadequate. In these cases, it is frequently combined with direct surgical excision (subcutaneous mastectomy) to ensure complete removal of the glandular tissue.
For severe cases involving significant skin redundancy (graded as Simon grade III or IV), simple excision may not suffice, and skin resection techniques similar to mastopexy may be required to remove excess skin and reposition the nipple-areola complex. Minimally invasive techniques, such as the use of an arthroscopic shaver or pull-through technique, allow for glandular removal through small incisions, minimising scarring. The choice of technique is tailored to the specific anatomical presentation of the patient to optimise aesthetic outcomes.
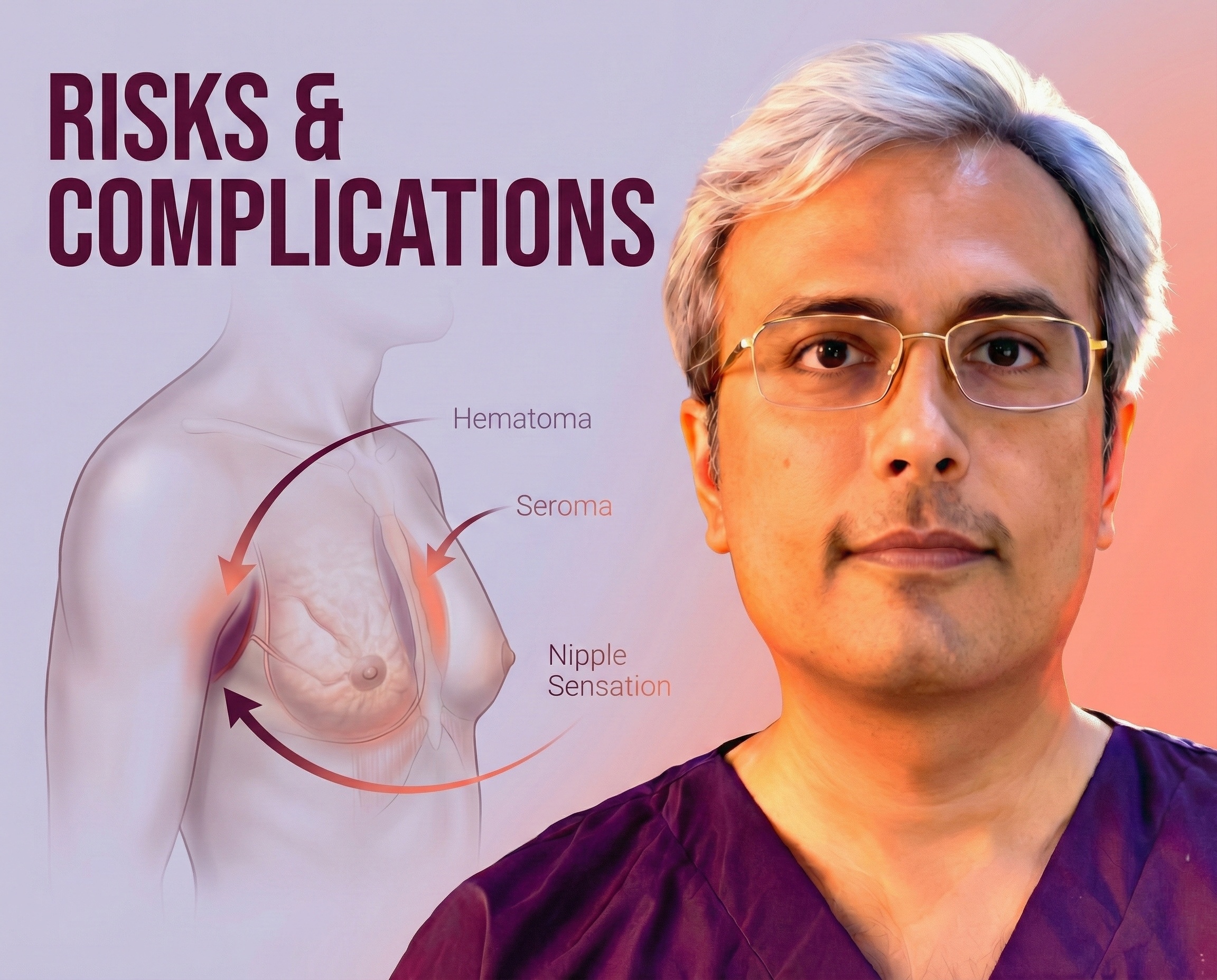
What should I expect during recovery, and what are the possible risks or complications after gynecomastia surgery?
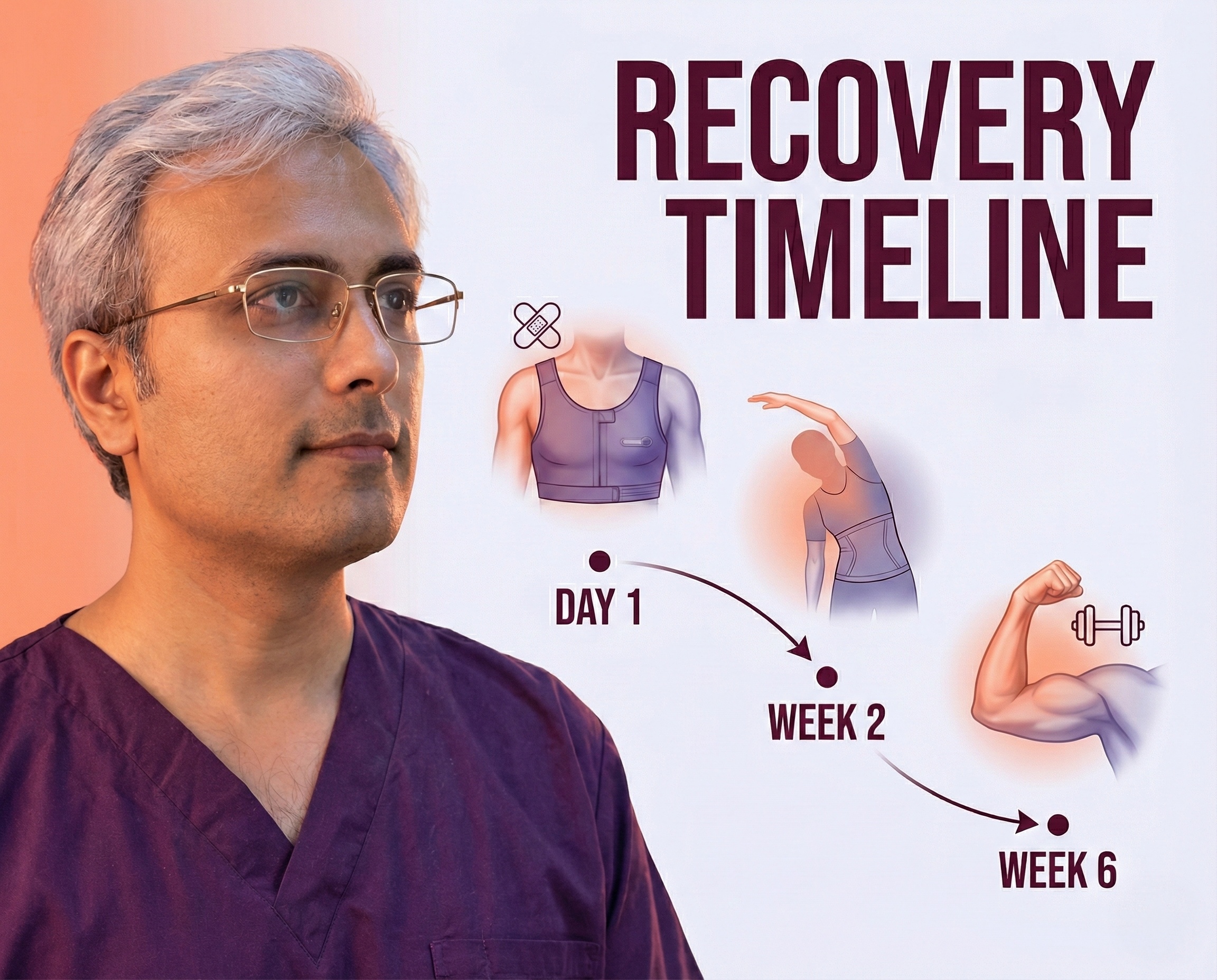
Recovery following gynecomastia surgery typically involves a period of reduced activity and the use of supportive garments. Patients are generally instructed to wear a compression garment for 4 to 6 weeks postoperatively to minimise swelling, prevent fluid accumulation, and help the skin retract and adhere to the chest wall. Most patients can return to light activities relatively quickly, but strenuous exercise, particularly involving the chest muscles, is usually restricted for several weeks to ensure proper healing.
Complications, while generally low, can occur. The most common early complication is hematoma formation, which is a collection of blood that may require surgical drainage. Seromas, or fluid collections, are also possible but can often be managed with aspiration. Infection is a risk with any surgery but is relatively infrequent in gynecomastia procedures. To mitigate these risks, some surgeons may utilise drains for a short period, although recent evidence suggests they may not always be necessary.
Aesthetic complications can include contour irregularities, asymmetry, or a “saucer deformity” caused by over-resection of the tissue deep to the nipple-areola complex. Changes in nipple sensation, either temporary or permanent numbness, can also occur. Scarring is inevitable with open excision but is typically well-concealed along the areolar border; however, hypertrophic or visible scarring remains a possibility, particularly in patients prone to keloids.
Overall, patient satisfaction with gynecomastia surgery is generally high, provided that realistic expectations are set. The procedure is considered safe, with a low rate of recurrence if the glandular tissue is adequately excised. Long-term follow-up usually shows stable results, with significant improvements in the patient’s quality of life and self-confidence.
Stop Guessing, Start Transforming
You don’t have to live with the discomfort or embarrassment of gynecomastia forever. If you suspect you have this condition, a simple consultation can provide the clarity you need.
Dr. Vishal Purohit is ready to help you reclaim your confidence with a safe, permanent, and customised treatment plan.
- 📞 Call/WhatsApp: +91 7718183535
- 📍 Visit Us: Kalpana Aesthetics, 2nd Floor, Jaipur Hospital, Mahaveer Nagar, Tonk Road, Jaipur
- 📅 Book Your Consultation Today
Disclaimer: The content provided in this blog post is for informational and educational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare provider or board-certified plastic surgeon regarding your specific medical condition. Dr Vishal Purohit is not liable for any decisions made based on this information.