When patients research Gynecomastia Surgery in Jaipur, they often get stuck on one question: “Do I need just liposuction, or do I need ‘the cut’?”
There is a common misconception that liposuction is the “modern” way and gland excision is the “old” way. This is false. They are two different tools for two different problems: Fat vs. Gland.
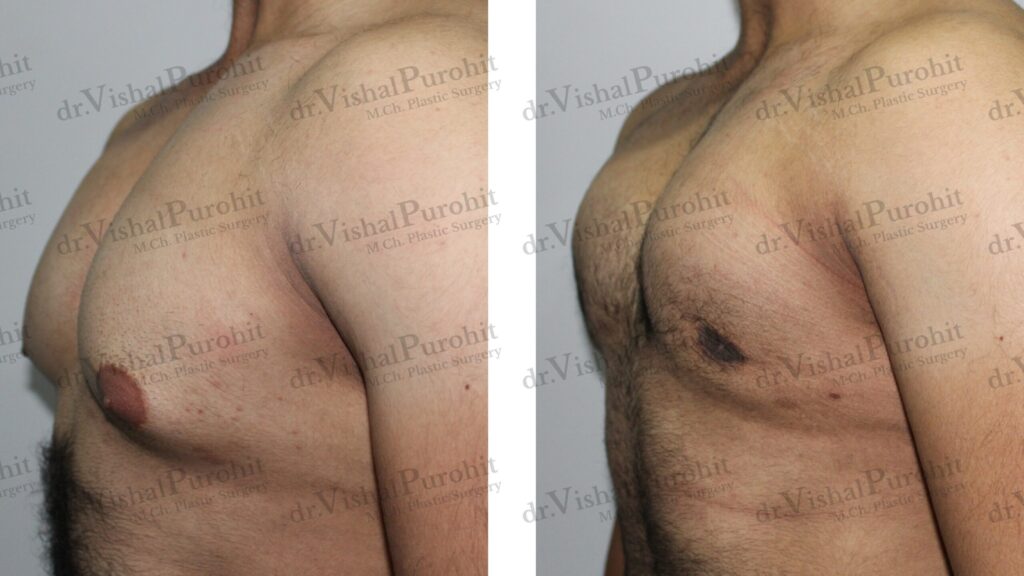
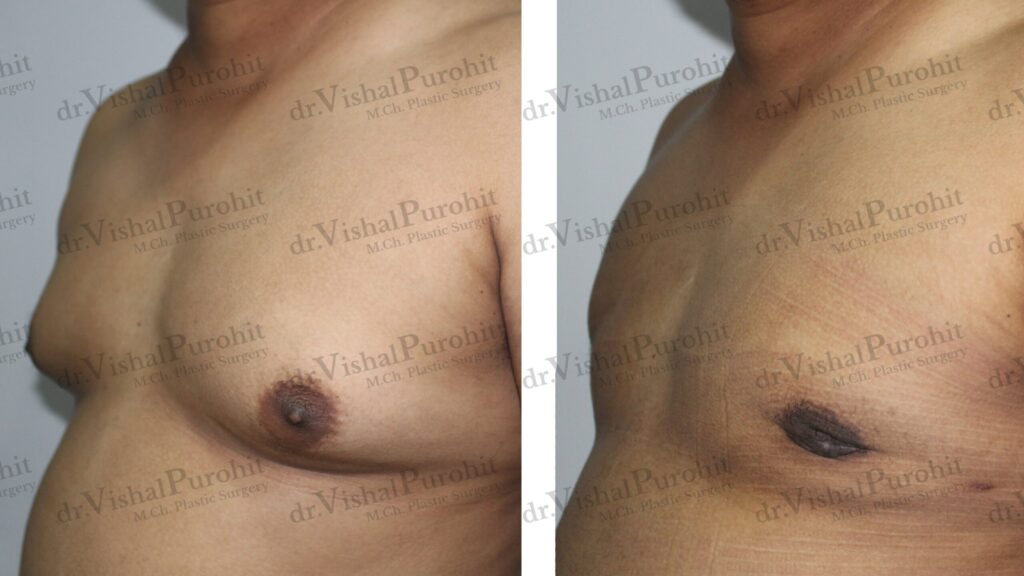
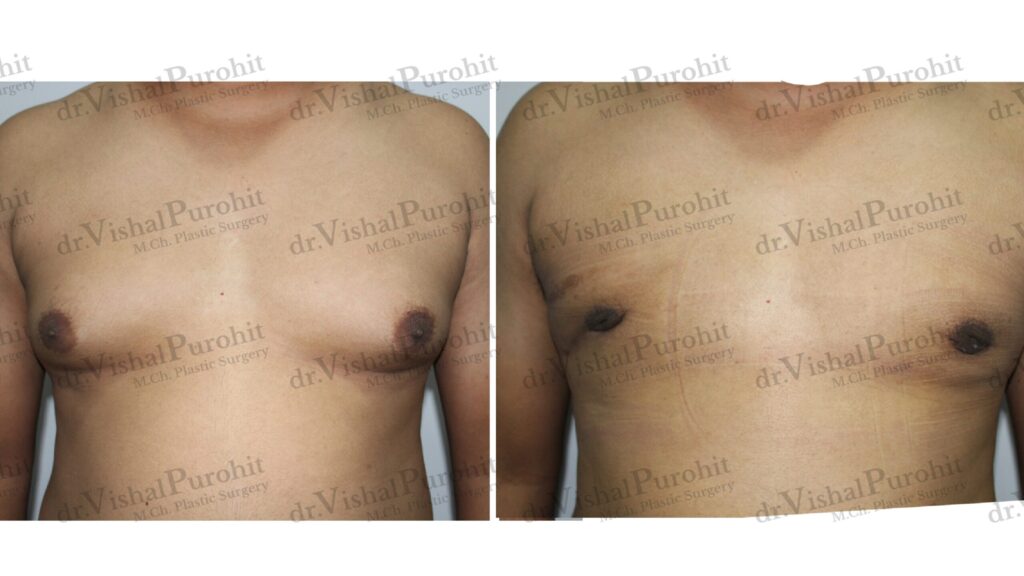
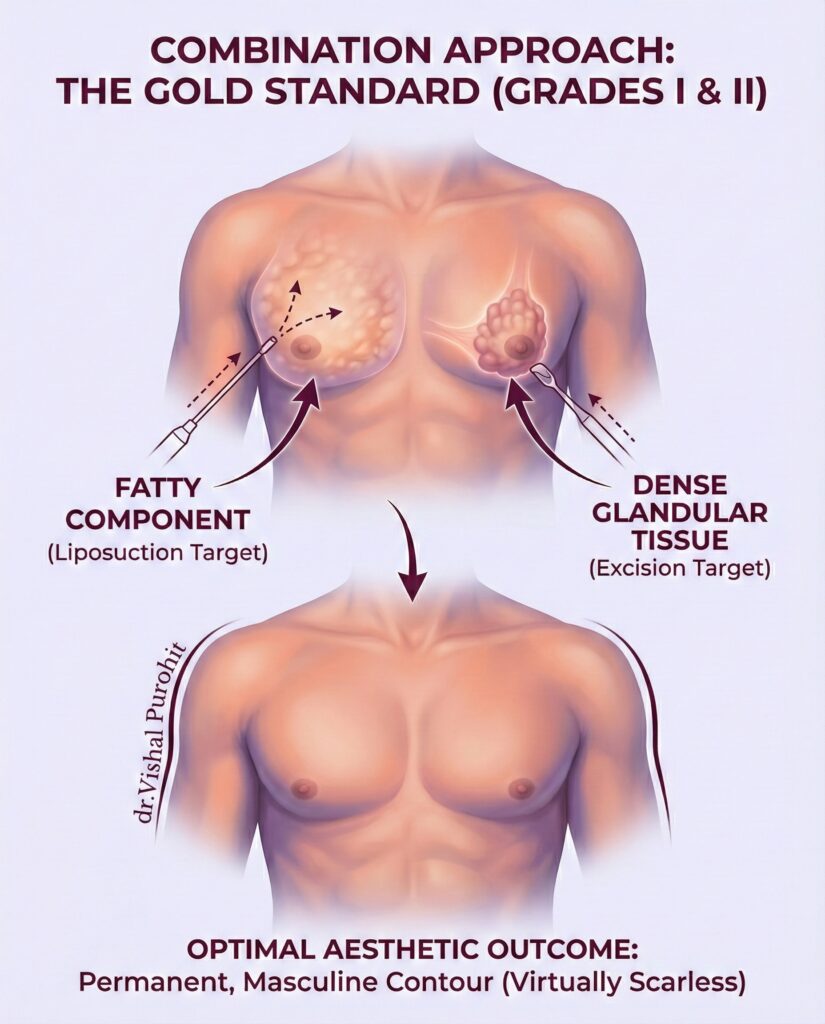
To achieve a truly sculpted, masculine chest, we often combine art with science. In this guide, I will break down the techniques we use to ensure your results are not just “flatter,” but anatomically correct.
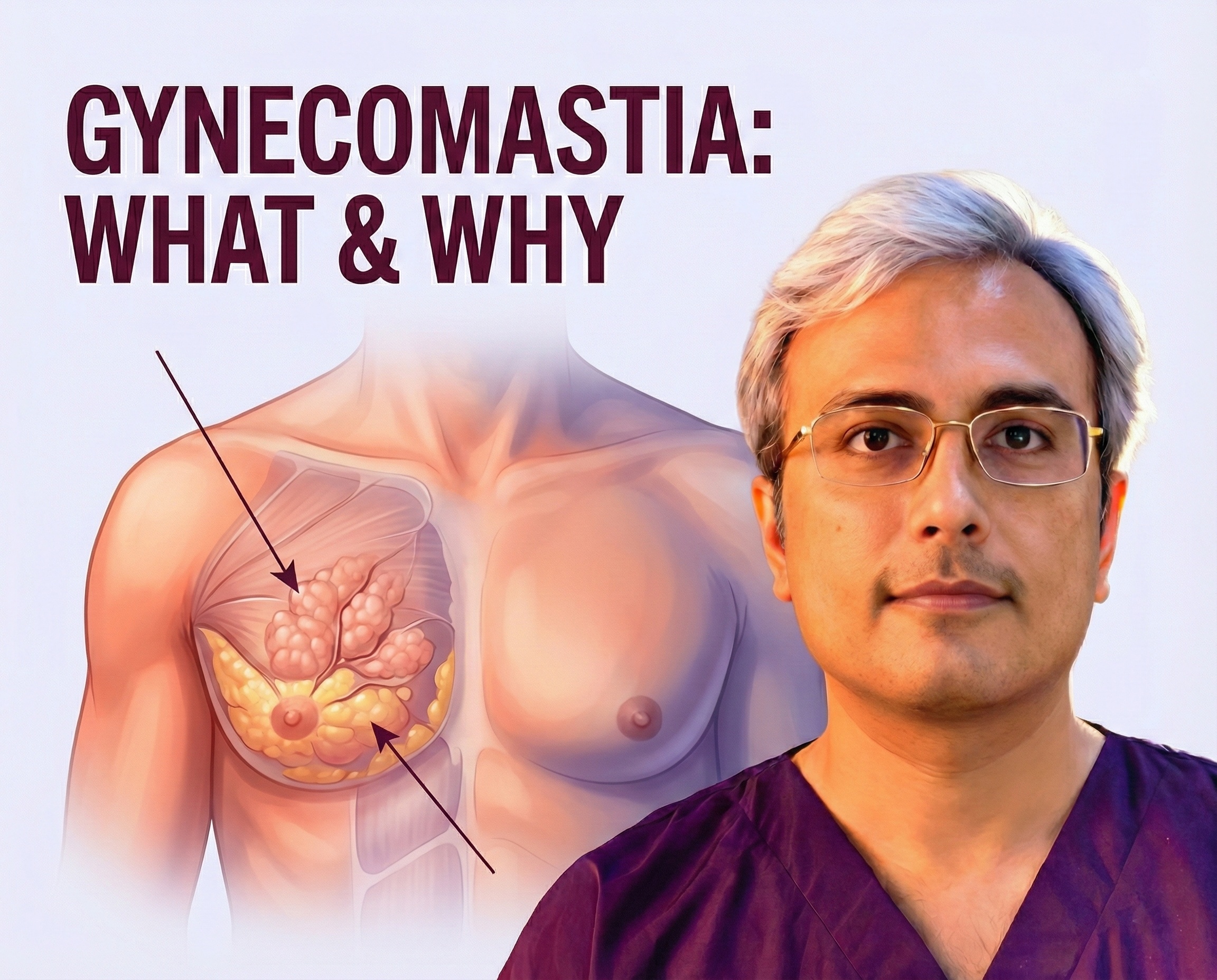
The Two Components of Gynecomastia
To understand the technique, you must understand the tissue. Most “man boobs” are a mix of two things:
- Adipose Tissue (Fat): Soft, squishy, and spread out.
- Glandular Tissue (The Gland): Firm, rubbery, and located directly behind the nipple.
The Golden Rule: Liposuction removes fat. Excision removes the gland.
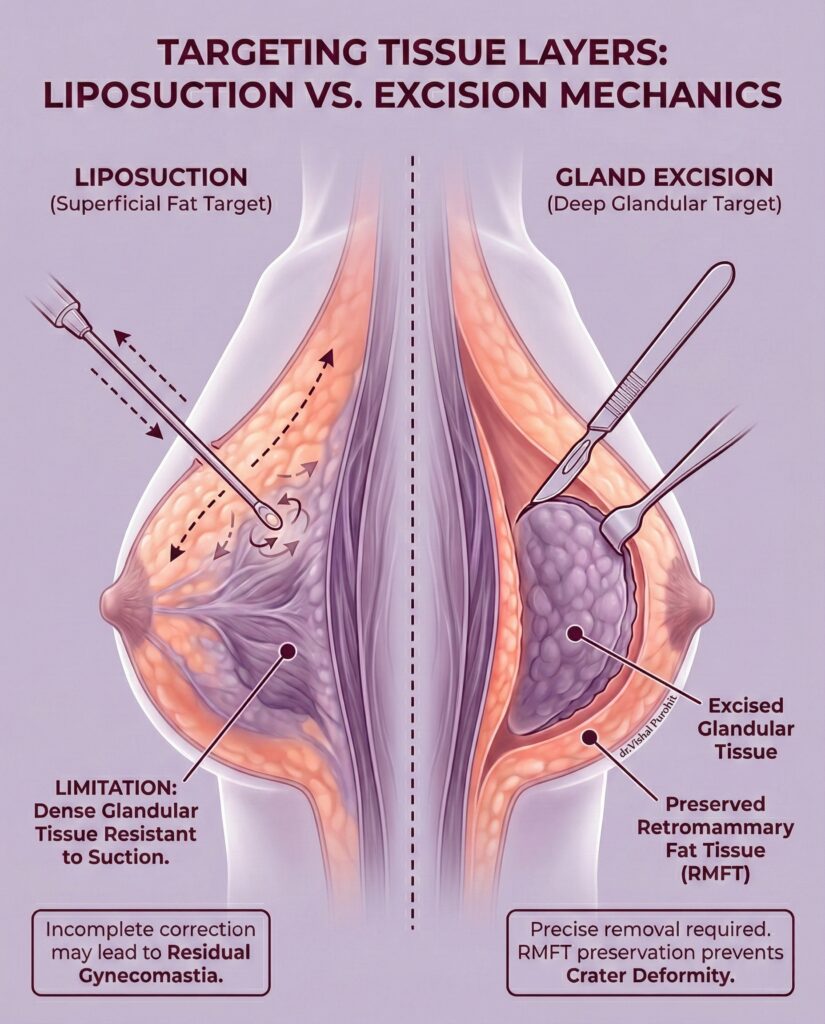
Liposuction: The Foundation of Contouring
Liposuction is almost always the first step. It allows us to debulk the chest and create a smooth taper towards the armpit (axilla).
How It Works
We use a thin tube (cannula) to suction out the fatty layer. This is excellent for defining the pectoral muscle borders.
- The Limitation: Liposuction cannot remove the hard, rubbery glandular disc. Attempting to force the gland out through a liposuction tube often leads to trauma or incomplete removal.
- Research Insight: Studies show that while pectoral high-definition liposculpture dramatically improves the chest contour, it is rarely sufficient on its own for true gynecomastia correction.
Surgical Excision: The “Gold Standard” for Gland Removal
If you have a puffy nipple or a hard lump, you almost certainly need surgical excision. This is the only way to physically remove the gland so it cannot grow back.
The Webster Technique (Gland Excision)
- The Incision: We make a tiny, semi-circular cut along the lower border of the areola. This location naturally hides the scar. (Worried about marks? Read our guide on Gynecomastia Scar Management).
- The Removal: The gland is carefully dissected from the muscle and skin and removed in one piece.
- The Importance: Medical literature confirms that direct excision is necessary for the treatment of gynaecomastia to prevent recurrence and ensure a flat nipple-areola complex.
Lipo vs. Surgery: Which One Do You Need?
This decision depends entirely on your specific anatomy and directly influences the Cost of Gynecomastia Surgery.
| Feature | Liposuction Only | Gland Excision (Open Surgery) | Combination (The Gold Standard) |
| Best For | Pseudo-gynecomastia (Fat only) | True Glandular Gynecomastia (Puffy Nipple) | Mixed Gynecomastia (Most Common) |
| Incision | Tiny Punctures (<4mm) | Periareolar (Hidden border) | Both |
| Recovery | 2-3 Days | 5-7 Days | 5-7 Days |
| Scarring | Minimal | Very Faint (Hidden) | Very Faint |
The Verdict: In my practice, 90% of patients require a combination of both. Liposuction flattens the chest wall, and excision removes the puffy nipple. Using only one often leads to dissatisfaction.
High-Definition Contouring: Beyond “Just Flattening”
Our goal isn’t just to make you flat; it’s to make you look fit.
We use clinical evaluation and management protocols to respect the aesthetic units of the chest. This means we don’t just scoop out tissue; we leave a thin layer of fat over the muscle to ensure a natural feel and prevent the nipple from sticking to the ribs (a “crater deformity”).
Patient Satisfaction
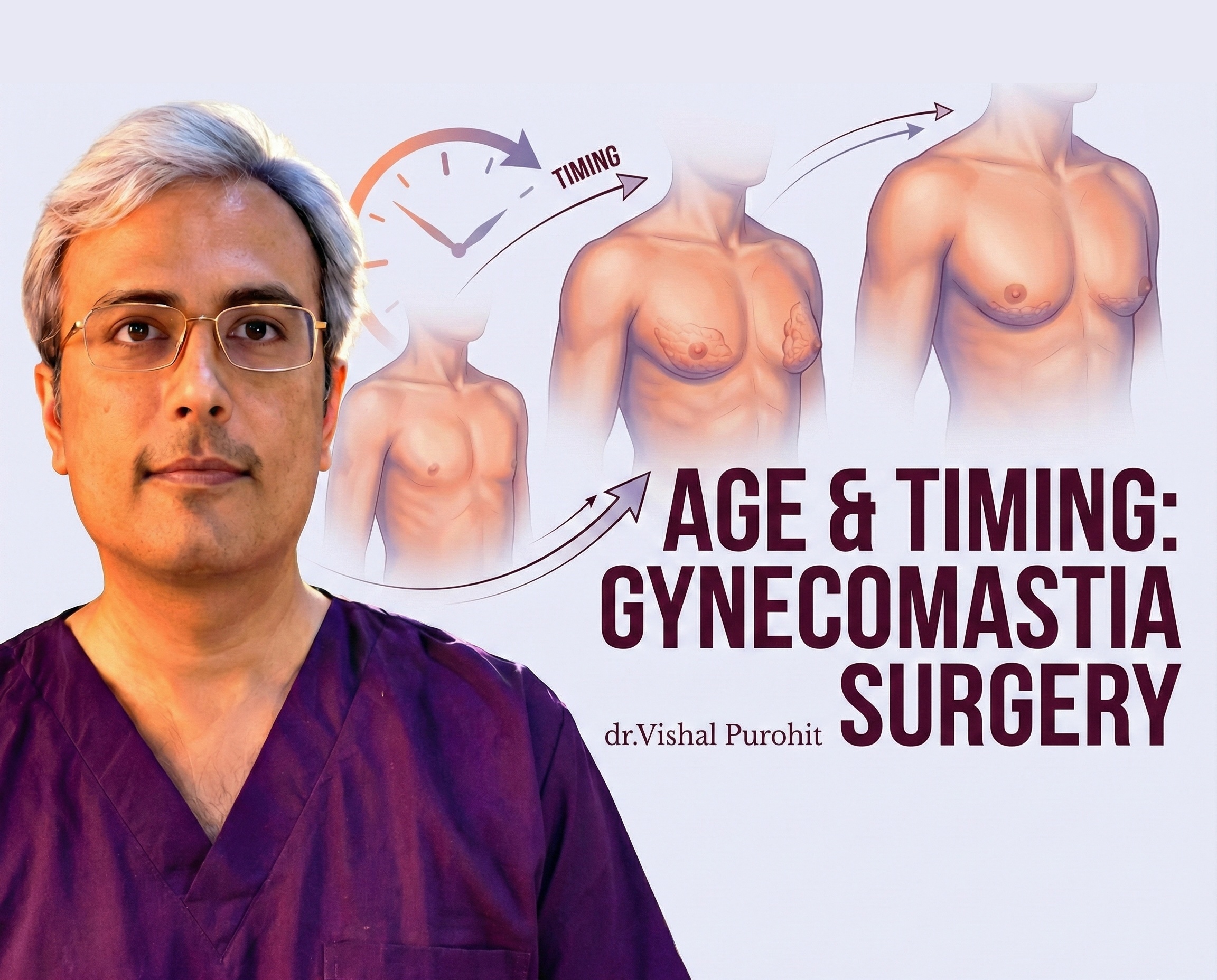
Choosing the right technique is the single biggest factor in happiness. Research confirms that tailoring the technique to the grade of gynecomastia leads to significantly higher patient satisfaction in gynecomastia treatment compared to using a single method for everyone.
Curious about the recovery time for these techniques? Check our Recovery Timeline Guide for Gynecomastia Surgery.
Ultimately, the complexity of the technique required—whether simple liposuction or complex gland excision—is a key factor in determining the final cost of the procedure.
Frequently Asked Questions
What surgical techniques are used to treat gynecomastia (liposuction, gland excision, or combined approaches)?
The surgical management of gynecomastia has evolved significantly from traditional open resections to less invasive methods that prioritise aesthetic outcomes. The standard approach often involves a subcutaneous mastectomy, which is the direct surgical removal of the glandular tissue, often performed through a periareolar incision. This technique is effective for removing the dense, fibrous breast disk that characterises true gynecomastia but carries risks of sensory changes and contour irregularities.
To address the fatty component of the breast and improve the overall chest contour, surgeons frequently utilise liposuction techniques. Conventional suction-assisted lipectomy (SAL) is commonly used, but advanced modalities like ultrasound-assisted liposuction (UAL) have gained popularity because they can selectively emulsify fat and disrupt fibrous tissue, making removal easier and stimulating skin retraction. Power-assisted liposuction (PAL) is another modality that reduces surgeon fatigue and facilitates the breakdown of dense tissue through an oscillating cannula.
In modern practice, a combined approach is frequently advocated as the gold standard for achieving the best aesthetic results. This involves using liposuction to contour the chest and remove adipose tissue, followed by a more limited excision of the remaining fibroglandular tissue, often using a pull-through technique to minimise incision size. This hybrid method allows for thorough removal of breast tissue while maintaining a smooth transition between the treated area and the surrounding chest wall.
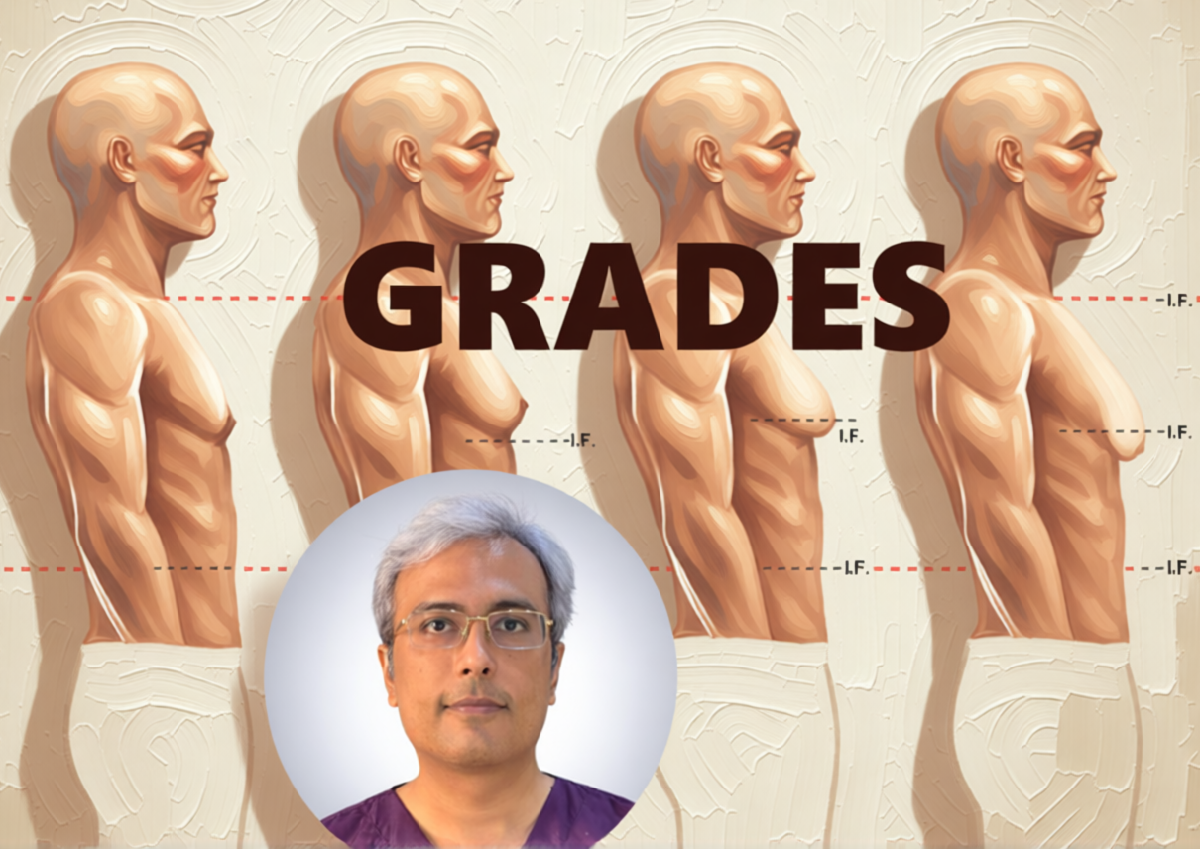
For more severe cases involving significant skin redundancy (Simon Grade III or IV), simple excision or liposuction may be insufficient. In these instances, skin-reduction techniques are required, such as a concentric periareolar excision (Benelli type) or more extensive reduction patterns like the inverted-T incision, to remove excess skin and reposition the nipple-areola complex. Additionally, newer minimally invasive instruments like the vacuum-assisted breast biopsy system and arthroscopic shavers are being explored to remove glandular tissue through tiny incisions.
How do you determine whether liposuction alone is sufficient or whether glandular excision is also necessary?
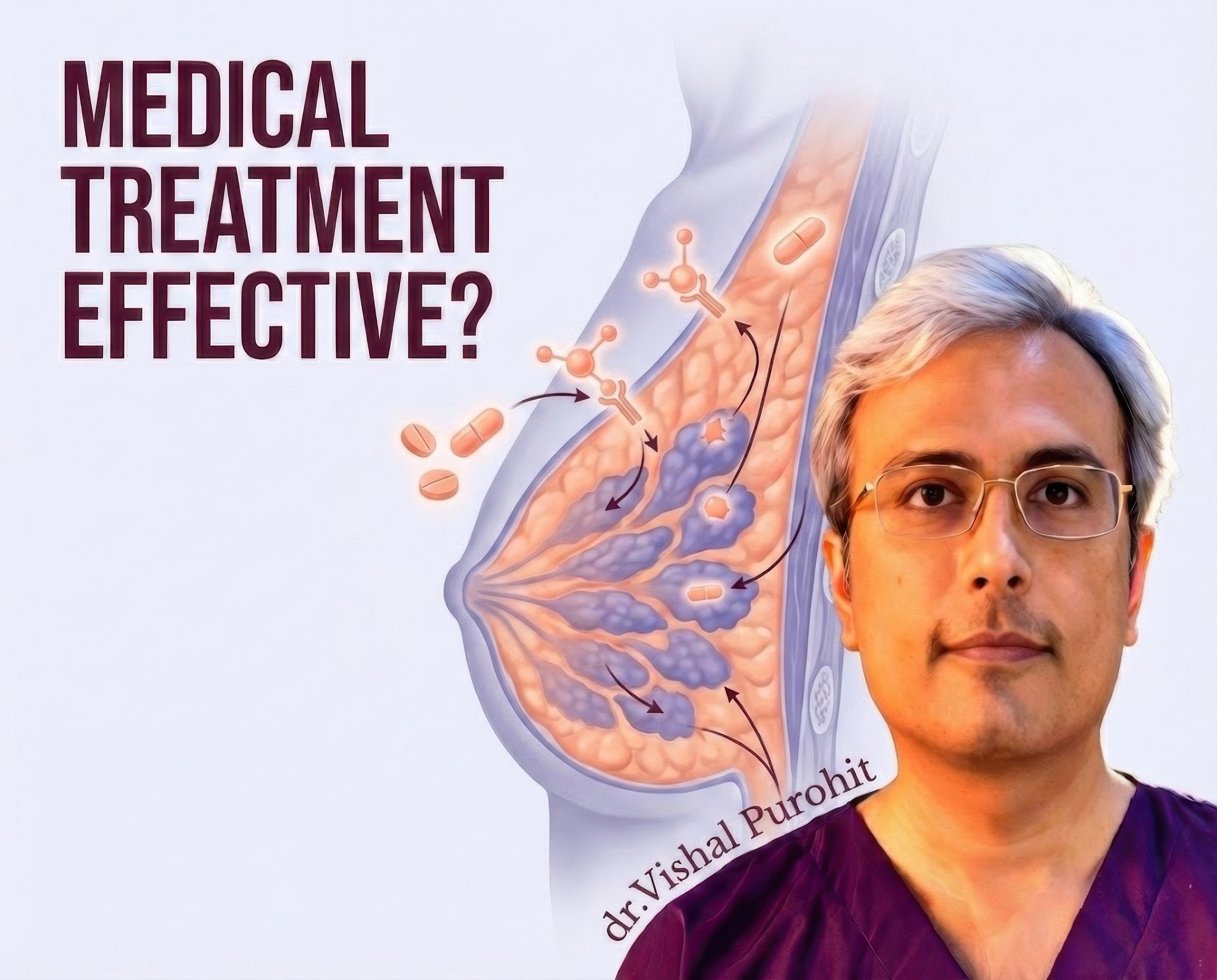
The decision to proceed with liposuction alone versus a combined approach depends largely on the composition of the breast tissue, which is assessed through physical examination and imaging. Patients with pseudogynecomastia, where the enlargement is primarily due to adipose tissue, are ideal candidates for liposuction combined with surgical excision, being unnecessary in purely fatty cases. However, true gynecomastia typically presents with a firm, rubbery disk of fibrous glandular tissue located directly beneath the areola, which is resistant to suction.
A “pinch test” is often utilised during the physical exam to estimate the ratio of fat to gland. If a distinct, palpable mass is felt, it indicates the presence of dense parenchyma that likely requires surgical excision, as liposuction cannulas have difficulty penetrating and removing this fibrous tissue. Conversely, if the breast consistency is soft and uniform with the surrounding fat, liposuction alone may be sufficient to achieve a flat chest contour.
Ultrasonography is a valuable diagnostic tool used to confirm the nature of the breast tissue before surgery. It helps differentiate between fatty and glandular components, allowing the surgeon to plan whether to use an open excision or a minimally invasive technique. Some surgeons advocate for the use of ultrasound-assisted liposuction even in fibrous cases, as the ultrasonic energy can help fragment the glandular tissue, potentially reducing the need for a large open incision, although a small pull-through excision is often still required to remove the remnant breast bud.
Ultimately, the goal is to prevent residual gynecomastia, which is a common cause of patient dissatisfaction if the glandular component is not adequately addressed. Studies have shown that treatment with liposuction alone resulted in a high percentage of residual tissue in patients with mixed or glandular gynecomastia, necessitating a secondary excision. Therefore, unless the condition is strictly fatty, a combined approach is generally recommended to ensure complete removal and prevent recurrence.
What incision locations and scarring can I expect with each surgical technique?
The location and extent of scarring are primary concerns for patients and depend heavily on the surgical technique employed. The standard open surgical approach typically utilises a semicircular periareolar incision, often placed along the inferior margin of the areola (Webster incision). This location is chosen to camouflage the scar at the junction of the darker areolar skin and the lighter chest skin, making it less conspicuous over time.
For liposuction-based procedures, the incisions are much smaller, typically 3 to 5 millimetres in length. These stab incisions are strategically placed to be hidden, such as in the axilla (armpit), the inframammary fold, or the lateral chest wall. A transaxillary incision is particularly favoured by some surgeons to avoid any scars on the anterior chest, although it requires specialised lighted retractors or endoscopic equipment to ensure complete gland removal.
In cases where the “pull-through” technique is used, the glandular tissue is removed through the same small incisions used for liposuction, or via a very small extension at the areolar border. This results in minimal scarring compared to a traditional open mastectomy. However, if the patient has significant skin redundancy (grade III or IV gynecomastia), more extensive skin-resection techniques may be required, such as a concentric “doughnut” excision around the areola or even an inverted-T pattern, which inevitably leaves more visible scars on the chest.
It is important to note that while periareolar incisions generally heal well, they can sometimes result in hypertrophy, hypopigmentation, or widening of the scar. To mitigate this, some surgeons use a zigzag periareolar incision to minimise scar visibility and prevent contracture. Regardless of the technique, the goal is always to keep the scars as inconspicuous as possible while allowing adequate access for tissue removal.
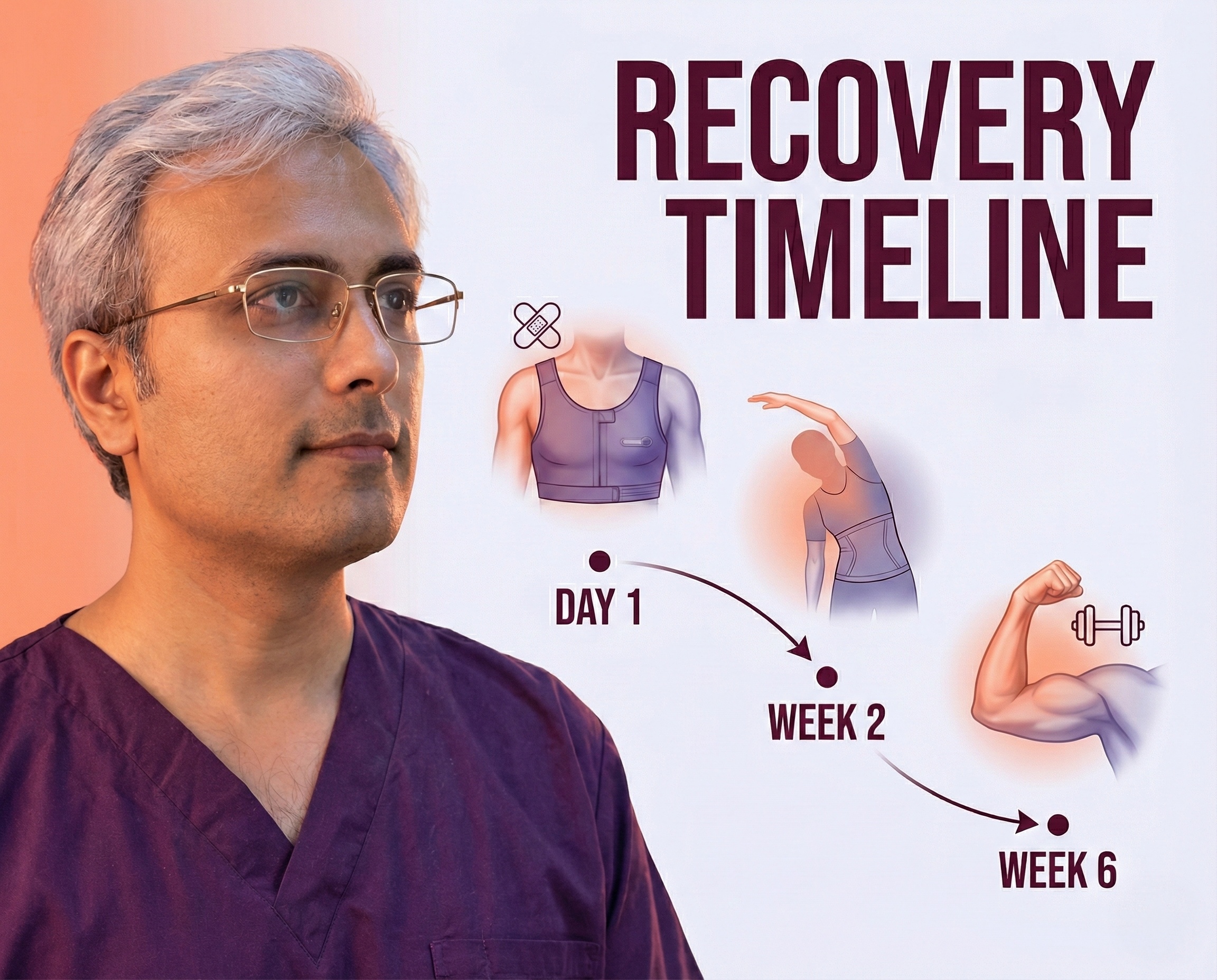
How does the chosen technique affect recovery time, pain, and return to exercise?
Recovery experiences can vary based on the invasiveness of the procedure. Patients undergoing minimally invasive procedures, such as those combining liposuction with a pull-through technique, generally experience a quicker recovery with less pain compared to extensive open excisions. The use of tumescent anesthesia, which involves infiltrating the tissue with a solution containing lidocaine and epinephrine, significantly reduces intraoperative bleeding and postoperative pain, often allowing the procedure to be performed on an outpatient basis without general anaesthesia.
The use of postoperative drains is a debated topic; while some surgeons use them to prevent fluid accumulation, recent studies suggest that suction drainage may not be necessary for routine gynecomastia surgeries and can be omitted to increase patient comfort without increasing complication rates. Instead, patients are typically required to wear a compression garment or vest for 2 to 6 weeks to minimise swelling, prevent seroma formation, and help the skin retract and adhere to the chest wall.
Return to normal activities and exercise is graduated. Patients are often advised to refrain from strenuous physical activity, particularly upper-body exercises, for about 3 to 4 weeks to prevent hematoma formation and ensure proper healing. For less invasive procedures, patients may return to work and light daily activities within a few days to a week.
Complications such as hematoma or seroma can prolong recovery. The incidence of these complications is generally low but can be higher in cases involving extensive glandular resection or in patients with high body mass index. Techniques that utilise external quilting sutures to close dead space have been shown to reduce the rate of hematoma formation, thereby potentially smoothing the recovery process.
Will the surgery or chosen technique change nipple sensation or the long-term chest contour?
Changes in nipple sensation are a potential risk of gynecomastia surgery, particularly with techniques that involve extensive dissection under the nipple-areola complex. Temporary hypoesthesia (reduced sensation) is relatively common but usually resolves within a few months as the nerves recover. However, aggressive resection or damage to the subdermal plexus during open excision can lead to permanent nipple sensation loss in a small percentage of patients.
The long-term chest contour is heavily influenced by the surgical technique and the amount of tissue removed. A common aesthetic complication is a “saucer deformity,” or a depression behind the nipple, caused by over-resection of the glandular tissue. To prevent this, surgeons typically leave a small, button-like disc of tissue (approximately 5-10 mm thick) attached to the undersurface of the areola to maintain projection and prevent adhesion to the pectoral muscle.
Conversely, under-resection can lead to residual fullness or recurrence, which is a frequent cause of patient dissatisfaction and revision surgery. Liposuction alone has a higher rate of incomplete removal if fibrous tissue is present, whereas open excision or combined techniques provide more reliable contouring. Long-term satisfaction is generally high, with studies showing significant improvements in self-confidence and quality of life, provided that the surgery successfully creates a masculine chest contour without significant irregularities.
Skin retraction is another critical factor for the final contour. While younger patients with elastic skin often achieve excellent results with volume reduction alone, older patients or those with significant weight loss may have residual skin laxity. In such cases, the chosen technique must account for skin management, potentially requiring staged procedures or skin-tightening technologies to avoid a deflated or sagging appearance.
Ready to Sculpt Your Chest?
Don’t guess which technique you need. A physical examination is the only way to know for sure if you have gland, fat, or both.
Dr. Vishal Purohit specialises in combination therapies to ensure the most natural, masculine result possible.
- 📞 Call/WhatsApp: +91 7718183535
- 📍 Visit Us: Kalpana Aesthetics, Jaipur
- 📅 Book Your Evaluation
Disclaimer: The content provided in this blog post is for informational and educational purposes only and does not constitute medical advice. Individual results vary. Always consult with a board-certified plastic surgeon.