Any surgeon who tells you a procedure has “zero risk” is not being honest with you. Every surgery, from wisdom tooth removal to heart surgery, carries some degree of risk.
However, gynecomastia surgery is statistically one of the safest cosmetic procedures performed today.
You deserve to know exactly what can go wrong, how likely it is, and what we do to prevent it. In this guide, we break down the safety profile of Gynecomastia Surgery in Jaipur with total transparency.
Minimising these risks begins with choosing a board-certified plastic surgeon who prioritises patient safety above all else
The Safety Data: What the Research Says
Gynecomastia surgery is classified as a “clean, elective procedure,” meaning it is performed on healthy individuals in a sterile environment.
Overall Complication Rate: A comprehensive review of outcomes indicates that the overall complication rate is low. Research on surgical management of gynecomastia suggests that major complications are rare when performed by qualified surgeons.
Patient Satisfaction: Despite minor risks, studies consistently show that surgical correction improves quality of life, with the vast majority of patients reporting high satisfaction with their physical and psychological outcomes.
Most Common Complications (And How We Prevent Them)
While major issues are rare, minor complications can occur. Here are the top three:
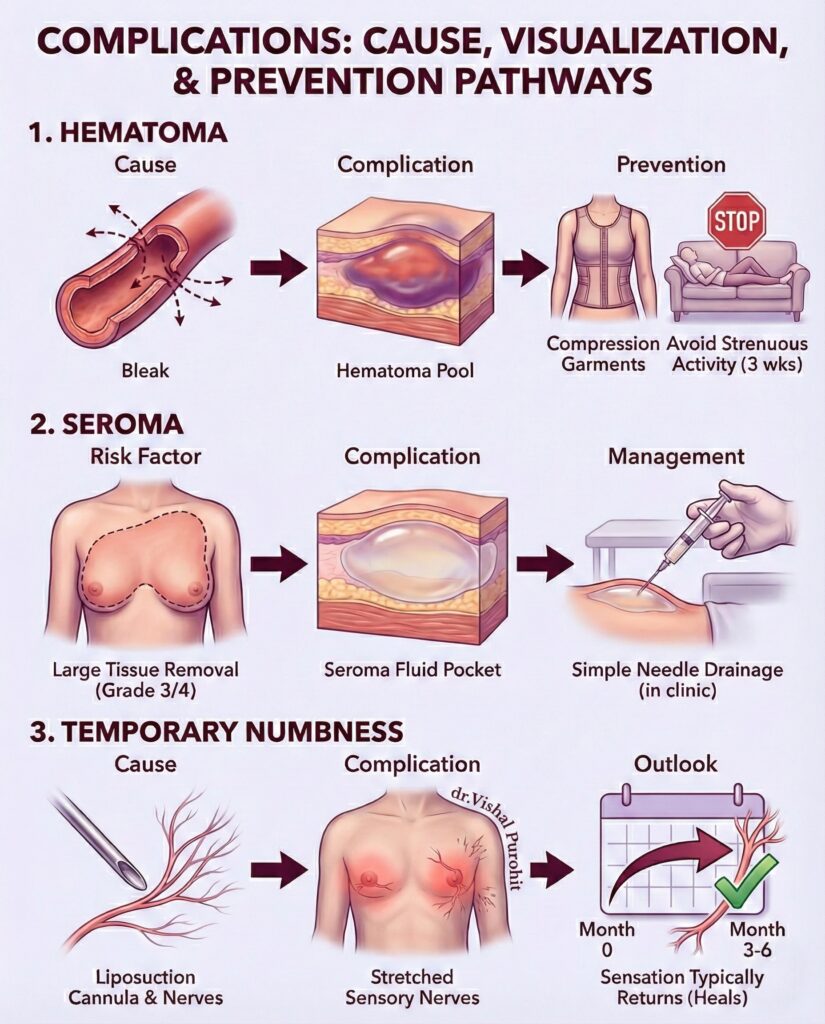
Hematoma (Collection of Blood)
This is the most common early complication. It happens when a small blood vessel leaks after surgery, causing a pool of blood to form under the skin.
The Data: Clinical studies have found that hematoma is the most frequent complication, though it is easily manageable if detected early.
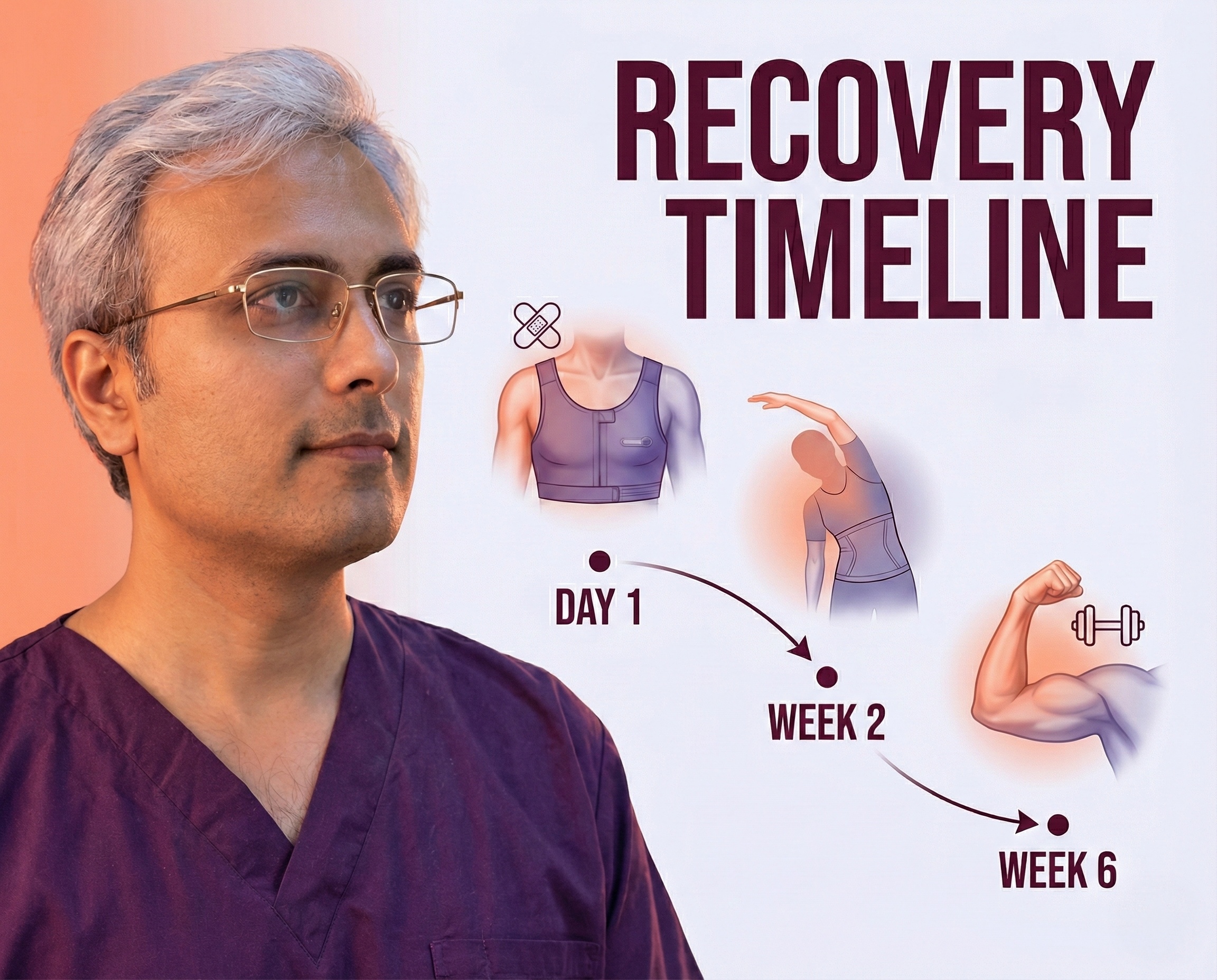
Prevention: We use Compression Garments immediately after surgery to collapse the space and stop bleeding. Patients are also advised to avoid strenuous activity for 3 weeks to prevent raising their blood pressure.
Seroma (Fluid Buildup)
A seroma is a pocket of clear fluid that can develop where tissue was removed. It typically resolves on its own or can be drained with a simple needle in the clinic.
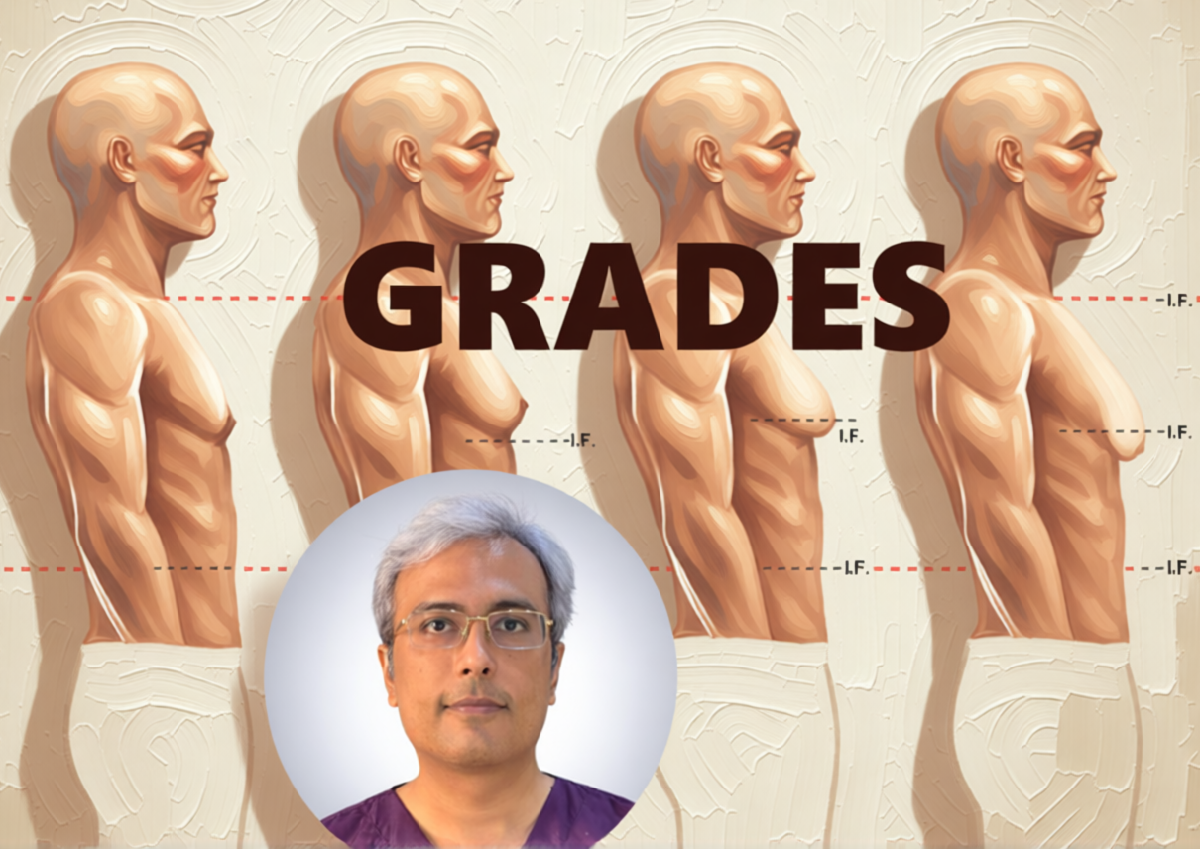
Risk Factors: It is slightly more common in Gynecomastia Grade 3 or Gynecomastia Grade 4 cases, where a large volume of tissue is removed. See our Gynecomastia Grades Guide.
Adhering strictly to your prescribed gynecomastia surgery recovery timeline and wearing your compression garment is the most effective way to prevent complications like seroma.
Temporary Numbness
It is normal to experience numbness or “pins and needles” in the nipple area. This is because tiny sensory nerves are stretched during liposuction.
Outlook: Sensation typically returns fully within 3 to 6 months as the nerves heal. Permanent loss of sensation is rare.
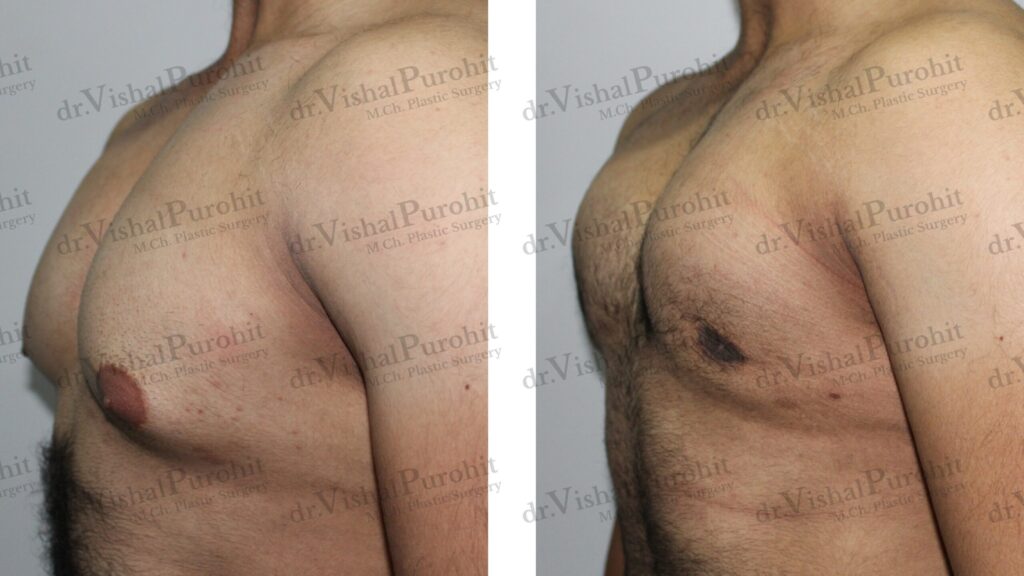
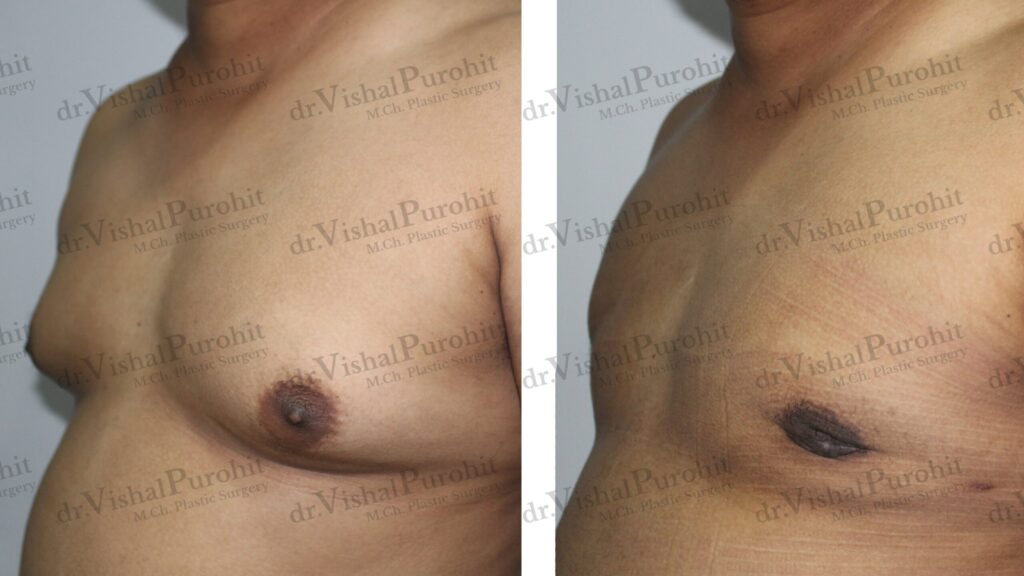
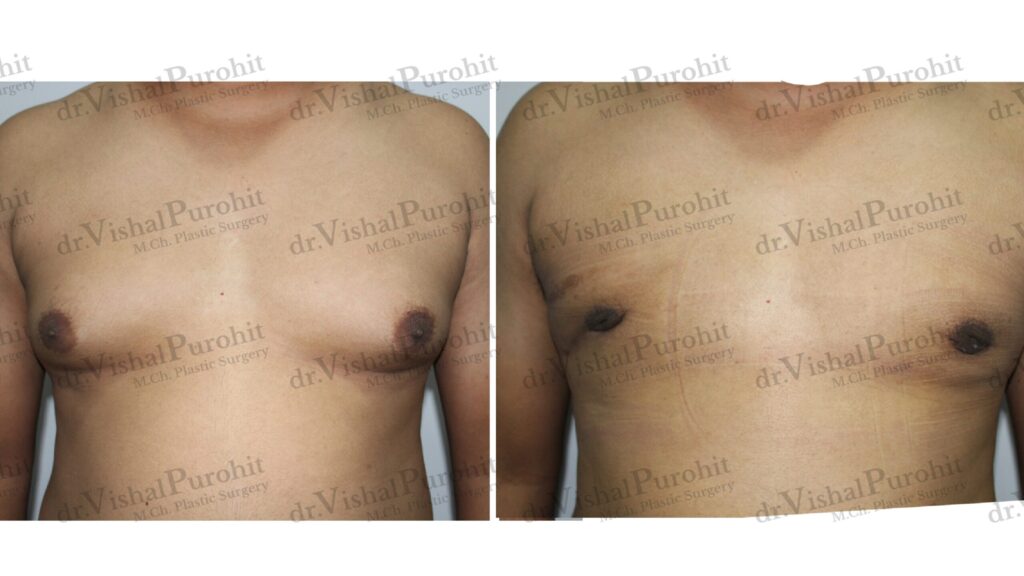
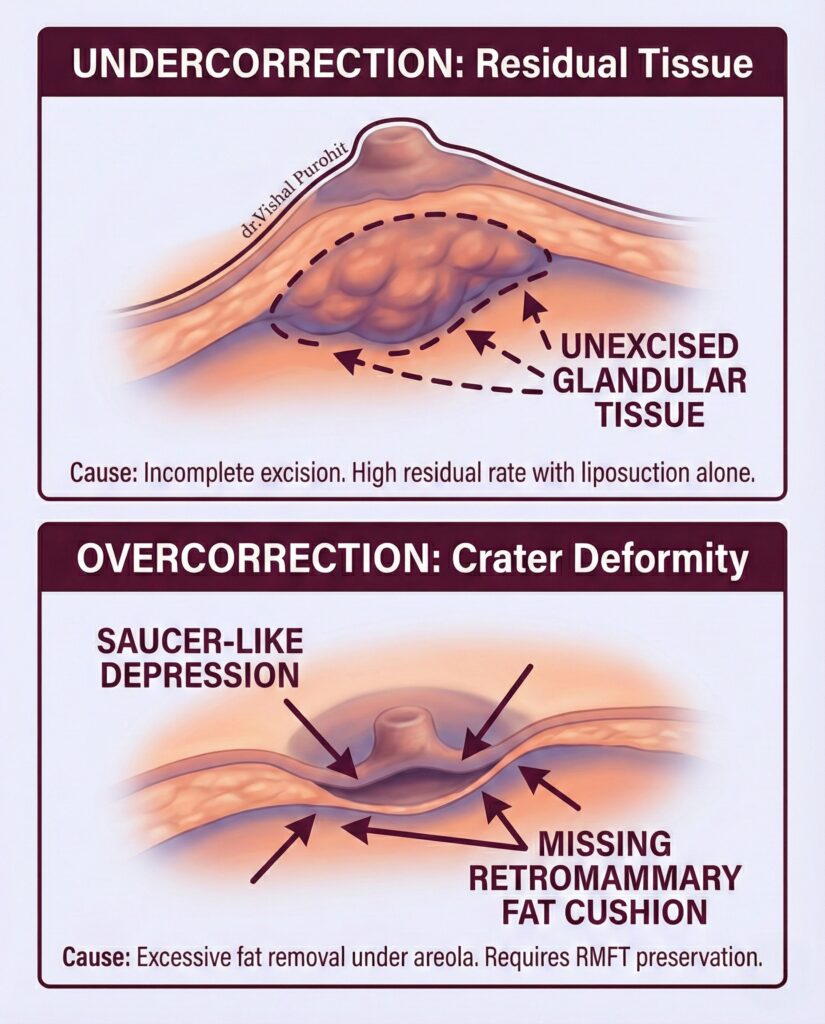
Aesthetic Risks: Contour Irregularities
The goal is a flat, smooth chest. However, aesthetic complications can happen if the surgery is not performed with precision.
- Crater Deformity: If too much gland is removed directly behind the nipple without leaving a small “cushion,” the nipple can cave in.
- Asymmetry: No two sides of the body are perfectly identical. While we aim for perfect symmetry, minor differences in shape may persist.
- Correction: Research indicates that while liposuction alone may lead to under-correction, combining it with gland excision significantly reduces the risk of contour deformities. Most minor issues can be fixed with a “touch-up” procedure after 6 months.
Scarring and Factors that Undermine Permanence
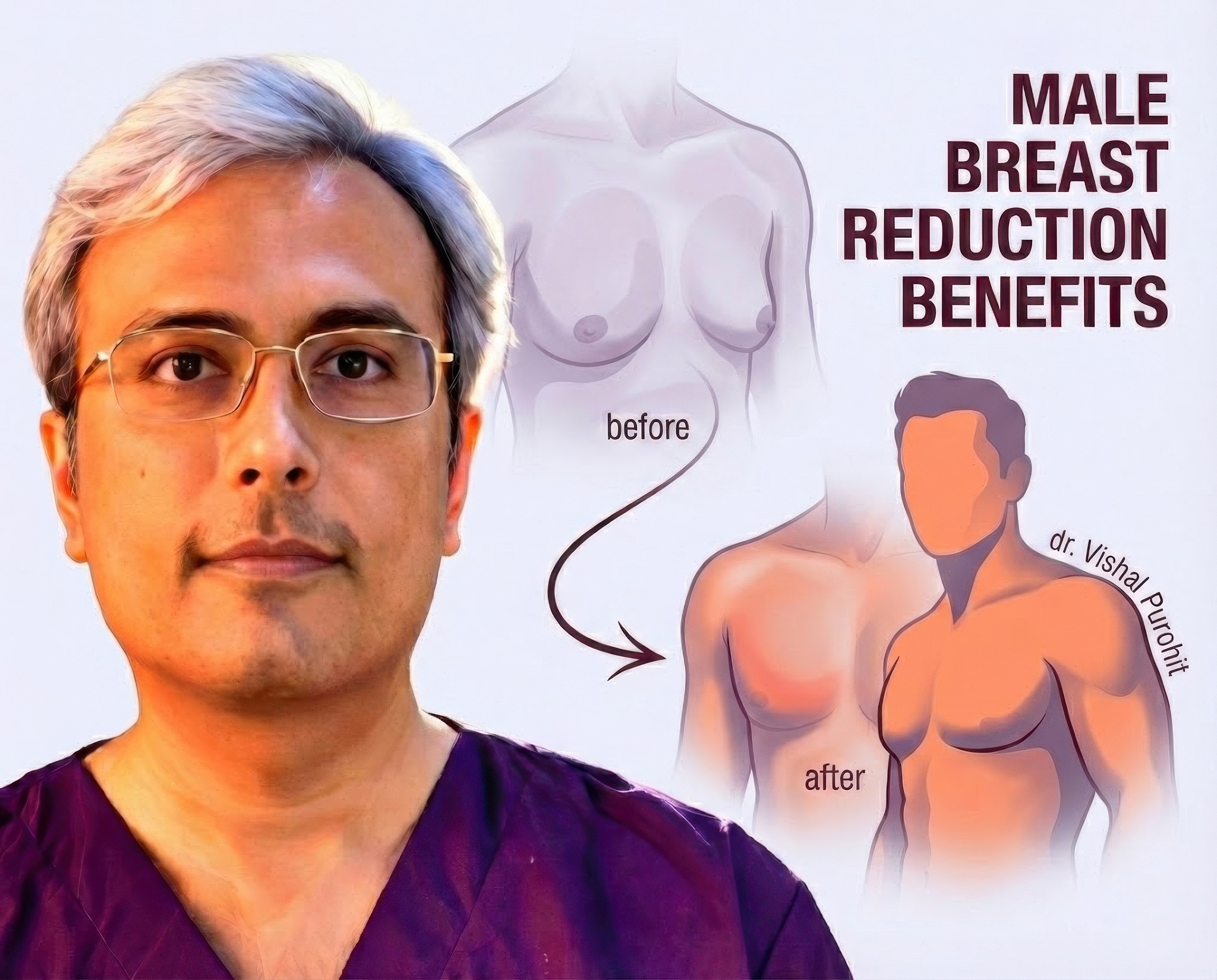
When committing to gynecomastia surgery, you seek a permanent solution that improves confidence. Our focus is on minimising visible scarring and educating you on the lifestyle choices necessary to ensure the results last.
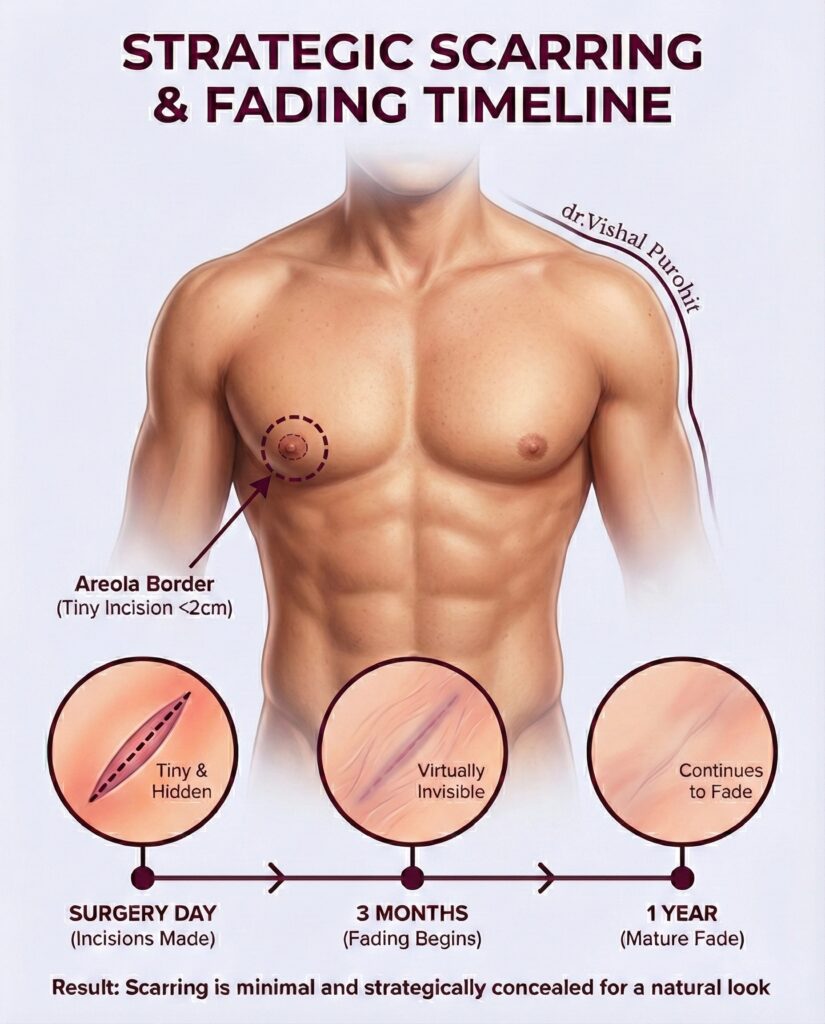
Scarring is Manageable and Strategic
Scars are a natural and inevitable outcome of any surgery. However, modern techniques are designed to ensure scarring is minimal and strategically concealed.
- Technique: Gynecomastia surgery can be a painless and virtually scarless method, often performed through tiny incisions (no more than 2cm). We cover this in detail in our guide to scarless confidence.
- Concealment: Incisions are placed in inconspicuous locations, like the border of the areola or on the lateral chest wall, ensuring no cut is visible on the front of the chest.
- Fading: Scars should fade considerably and become virtually invisible in 3 months, continuing to fade for 1 year.
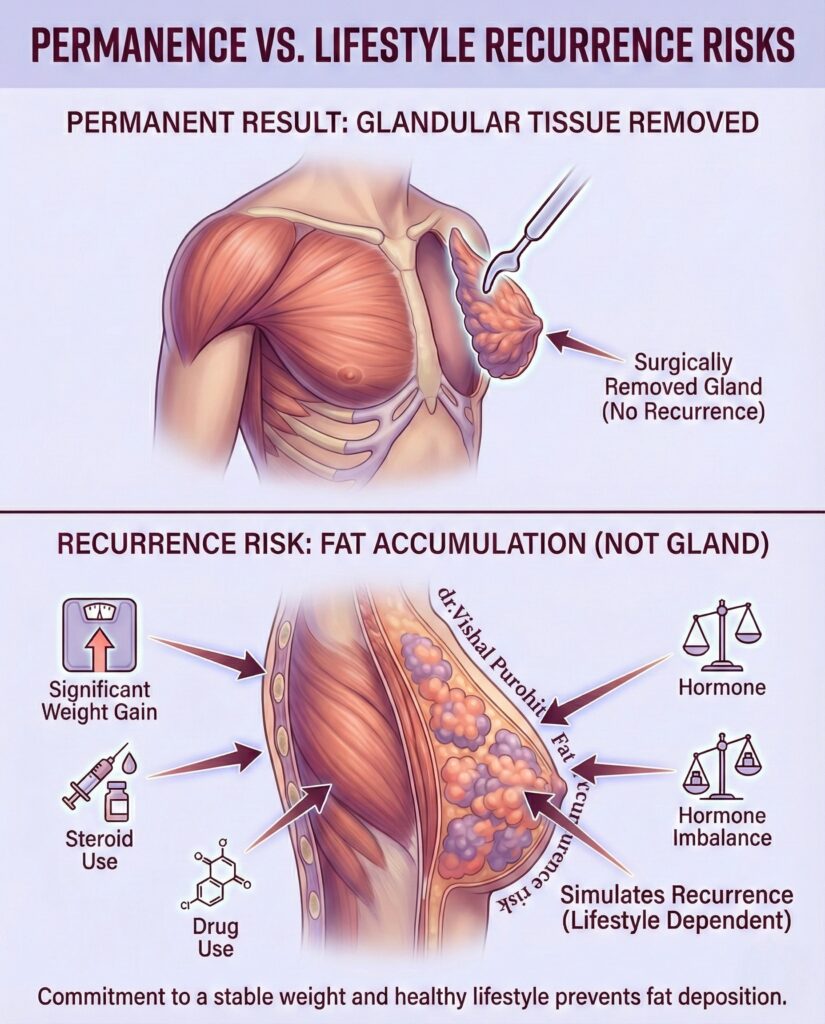
Avoiding Recurrence Requires Commitment
The great news is that the results of gynecomastia surgery are permanent because the glandular tissue is surgically removed.
However, recurrence may occur if you do not maintain a healthy lifestyle. This recurrence is not gynecomastia but fat accumulation, which simulates the look and feel of recurrence.
- Recurrence Causes: Recurrence can be triggered by significant weight gain, steroid use, drug use, or a hormone imbalance – all resulting in fat accumulation.
- Lifestyle Management: You must maintain a stable weight. If the gynecomastia was caused by substance use, you must stop using the substance to avoid recurrence due to fat deposition.
Anaesthesia Safety: Local vs. General
Many patients are anxious about “going under.”
- Local Anaesthesia: For Grade 1 and 2 cases, we often use Tumescent Local Anaesthesia. You remain awake but feel no pain. This eliminates the risks associated with general sedation.
- General Anaesthesia: For larger cases (Grade 3 & 4), general anaesthesia is safer as it protects your airway.
- Safety Record: Modern anaesthesia is incredibly safe. Monitoring equipment tracks your heart, oxygen, and blood pressure every second.
Reducing Your Risk: The Patient’s Role
Safety is a partnership. You can significantly lower your risk of complications by following these rules:
- Stop Smoking: Nicotine kills skin. You must stop smoking 3 weeks before and after surgery to prevent nipple necrosis (tissue death).
- Avoid Blood Thinners: Discontinue aspirin, Vitamin E, and fish oil 10 days prior to surgery to reduce the risk of hematoma.
- Wear Your Vest: The compression garment is your “second skin.” Wearing it 24/7 for the first 4 weeks is the #1 way to prevent fluid buildup.
Frequently Asked Questions
What are the common risks and complications associated with gynecomastia surgery?
The most common risks associated with gynecomastia surgery are minor and treatable, including hematoma (a collection of blood), seroma (fluid accumulation), and temporary changes in nipple sensation.
While serious complications are rare, the procedure carries inherent risks like any surgery. Common localised issues include hematoma, seroma, infection, and contour irregularities. A hematoma is a collection of blood under the skin that may require drainage, while a seroma is a fluid buildup that can often be managed with aspiration or compression. Aesthetic risks include asymmetry between the two sides or a “saucer deformity” if too much tissue is removed from behind the nipple.
Systemic risks, such as reactions to anaesthesia or thromboembolism, are extremely uncommon in healthy patients but must be screened for. To mitigate aesthetic risks like irregularities or skin redundancy, we often employ advanced techniques; for example, concentric skin reduction can be used in higher-grade cases to manage excess skin without leaving large scars.
As your surgeon, I prioritise minimising these risks through precise technique and patient selection. We know that complications like hematoma are often related to the extent of dissection and the patient’s blood pressure control; by using external quilting sutures to obliterate dead space, we can significantly reduce the expansion of any potential hematoma. My goal is to ensure you achieve a masculine chest without trading one aesthetic problem for another.
If you are concerned about specific risks based on your medical history, please schedule a consultation so we can discuss a personalised safety plan.
How likely is it to experience infection or bleeding after gynecomastia surgery?
Bleeding (hematoma) is the most frequent early complication, occurring in roughly 2-6% of cases, while infection is extremely rare when proper sterile techniques and antibiotics are used.
Hematoma formation is generally the most common immediate complication, reported in varying rates depending on the technique and patient population. For example, studies have shown a postoperative hematoma rate of approximately 5.8% in open excision cases, though this drops significantly with less invasive techniques. Infections are very uncommon; in a large analysis of pediatric and adult cases, surgical site infection rates were found to be as low as 0.5% to 1.3%.
To further reduce the risk of bleeding, we advise avoiding blood thinners and supplements before surgery. In specific high-risk populations, such as bodybuilders using anabolic steroids, the risk of hematoma requiring evacuation may be slightly higher due to increased vascularity, necessitating meticulous hemostasis during the procedure. Using compression garments post-surgery also helps control swelling and prevent fluid collection.
In my practice in Jaipur, we adhere to strict sterile protocols to keep infection rates near zero. We also focus on the gentle handling of tissues to prevent bleeding. Understanding your specific risk profile allows us to take extra precautions, ensuring your recovery is smooth and uneventful.
If you have a history of bleeding disorders or are taking medications that affect blood clotting, please disclose this during your consultation so we can prepare accordingly.
Can gynecomastia surgery affect nipple sensation or chest contour permanently?
Temporary numbness or changes in sensation are common but usually resolve over time; however, permanent sensory loss or significant contour deformities like a “saucer” depression are rare with experienced surgeons.
Changes in nipple sensation, such as prolonged hypesthesia (numbness), can occur in up to 25% of cases but typically recover spontaneously within a few months. Permanent loss is uncommon and is often related to the extent of the surgery. Regarding contour, over-resection of the glandular tissue directly behind the nipple can lead to a saucer deformity or depression. Conversely, under-resection can leave residual fullness.
To prevent contour irregularities and preserve sensation, we often leave a small disc of tissue (roughly 5-10mm) beneath the nipple-areola complex to maintain blood supply and support. Advanced techniques, such as the pull-through technique used in conjunction with ultrasonic liposuction, allow us to precisely remove fibrous tissue while minimising trauma to the surrounding sensory nerves.
I believe that preserving the natural feel and look of the chest is just as important as reducing its size. By carefully sculpting the chest rather than just removing tissue, we aim to maintain sensation and create a smooth, masculine profile that looks natural even when you are shirtless.
To discuss the specific techniques we use to protect nipple sensation and ensure a smooth contour, book an appointment for an assessment.
What signs after surgery should prompt me to contact my surgeon?
You should contact us immediately if you experience excessive swelling on one side (indicating a hematoma), shortness of breath, chest pain, or signs of infection such as fever and pus-like drainage.
While recovery is usually straightforward, vigilance is key. A rapidly expanding swelling, particularly on just one side, is a classic sign of a hematoma that may require drainage. In rare cases, partial nipple necrosis can occur if the blood supply is compromised, appearing as dark or dusky skin on the nipple.
You must also watch for systemic signs. Although extremely rare, symptoms like shortness of breath or chest pain could indicate a thromboembolic event. Additionally, persistent redness, warmth, or fluid drainage from the incision sites could indicate a breast abscess or infection, which needs immediate antibiotic treatment.
Your safety extends beyond the operating room. We provide 24/7 support for our patients because catching a complication early—like a small hematoma or early infection—makes it easily manageable. Never hesitate to call; it is always better to be safe.
If you notice any unusual symptoms after your surgery, do not wait for your scheduled follow-up; contact our clinic immediately for guidance.
Are there ways to minimise the risk of complications before and after gynecomastia surgery?
Yes, strictly following pre-operative guidelines like quitting smoking and avoiding blood thinners, along with wearing post-operative compression garments, significantly minimises complication risks.
Preparation is your best defence against complications. You must cease smoking and nicotine use for at least 6 weeks before and after surgery to prevent wound healing problems and infection. Additionally, avoiding aspirin and anti-inflammatory drugs reduces the risk of bleeding. During the procedure, the use of external quilting sutures can help obliterate dead space and minimise hematoma formation.
Post-operatively, adherence to care instructions is vital. We often forego closed-suction drains in standard cases to reduce discomfort and scarring, relying instead on compression garments to manage swelling and prevent fluid buildup. Wearing your compression garment as directed ensures the skin retracts smoothly and fluid does not accumulate.
I view surgery as a partnership. My team and I provide the technical expertise and a sterile environment, but your commitment to the pre- and post-operative guidelines is what ultimately secures a complication-free recovery and a perfect result.
To get a full checklist of how to prepare for your surgery and ensure the safest possible experience, please visit us for a consultation.
Trust in Transparency
At Kalpana Aesthetics, we don’t hide the risks; we manage them. Dr. Vishal Purohit’s complication rate is well below the national average because of his meticulous surgical technique and strict safety protocols.
If you are ready to discuss your safety and results in person, book a consultation today.
- 📞 Call/WhatsApp: +91 7718183535
- 📍 Visit Us: Kalpana Aesthetics, Jaipur
- 📅 Book Your Safety Consultation
Disclaimer: The content provided in this blog post is for informational and educational purposes only and does not constitute medical advice. Individual risks vary based on health history. Always consult with a board-certified plastic surgeon.